调查孕妇患心肌病的风险因素。
IF 3.2
2区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
背景:妊娠期心肌病严重影响产妇健康,导致高发病率和高死亡率。识别这种疾病的风险因素对于加强产前护理和预防不良后果至关重要:这项基于人群的病例对照研究调查了与孕妇心肌病相关的风险因素:我们分析了 2017 年 3 月 1 日至 2024 年 6 月 20 日期间在马什哈德医科大学附属医疗机构接受治疗的 5133 名孕妇(1686 例患有心肌病,3447 例对照组未患有心肌病)的数据。风险因素通过逻辑回归模型进行评估,该模型计算了各种人口统计学、医学和妊娠相关变量的调整后几率比(AORs)及95%置信区间(CIs):结果:妊娠期心肌病的重要风险因素包括肥胖(AOR = 2.11,95 % CI:1.43-2.02)、教育程度较高(AOR = 1.84,95 % CI:1.25-1.86)、精神健康问题(AOR = 2.07,95 % CI:1.7-2.5)、家庭暴力(AOR = 2.02,95 % CI:1.08-3.6)、双胎妊娠(AOR = 2.6,95 % CI:1.57-4.6)和先兆子痫(AOR = 6.9,95 % CI:2.78-17.4)。其他风险因素包括缺乏体能(AOR = 1.5,95 % CI:1.13-2.007)、孕期传染病史(AOR = 1.4,95 % CI:1.11-1.76)、贫血(AOR = 1.57,95 % CI:1.15-2.09)和高血压(AOR = 1.55,95 % CI:1.18-2.02)。吸烟会增加风险,但无统计学意义(AOR = 1.29,95 % CI:0.69-2.4):结论:在产前护理中解决可改变和不可改变的风险因素对于降低心肌病发病率和改善孕产妇心血管健康至关重要。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Investigating the risk factors of cardiomyopathy in pregnant mothers
Background
Cardiomyopathy during pregnancy significantly impacts maternal health, contributing to high morbidity and mortality. Identifying risk factors for this condition is crucial for enhancing prenatal care and preventing adverse outcomes.
Study design
This population-based case-control study investigates the risk factors associated with cardiomyopathy in pregnant women.
Methods
We analyzed data from 5133 pregnant women (1686 cases with cardiomyopathy and 3447 controls without cardiomyopathy) who received care at healthcare facilities affiliated with Mashhad University of Medical Sciences between March 1, 2017, and June 20, 2024. Risk factors were assessed through logistic regression models, which calculated adjusted odds ratios (AORs) with 95 % confidence intervals (CIs) for various demographic, medical, and pregnancy-related variables.
Results
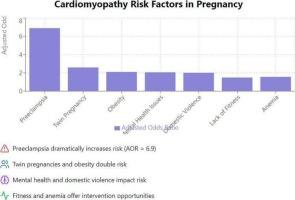
Significant risk factors for cardiomyopathy in pregnancy included obesity (AOR = 2.11, 95 % CI: 1.43–2.02), higher education level (AOR = 1.84, 95 % CI: 1.25–1.86), mental health issues (AOR = 2.07, 95 % CI: 1.7–2.5), domestic violence (AOR = 2.02, 95 % CI: 1.08–3.6), twin pregnancy (AOR = 2.6, 95 % CI: 1.57–4.6), and preeclampsia (AOR = 6.9, 95 % CI: 2.78–17.4). Additional risk factors included lack of physical fitness (AOR = 1.5, 95 % CI: 1.13–2.007), history of infectious disease during pregnancy (AOR = 1.4, 95 % CI: 1.11–1.76), anemia (AOR = 1.57, 95 % CI: 1.15–2.09), and hypertension (AOR = 1.55, 95 % CI: 1.18–2.02). Smoking increased risk but was not statistically significant (AOR = 1.29, 95 % CI: 0.69–2.4).
Conclusion
Addressing modifiable and non-modifiable risk factors in prenatal care is crucial to reducing cardiomyopathy incidence and improving maternal cardiovascular health.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

International journal of cardiology
医学-心血管系统
CiteScore
6.80
自引率
5.70%
发文量
758
审稿时长
44 days
期刊介绍:
The International Journal of Cardiology is devoted to cardiology in the broadest sense. Both basic research and clinical papers can be submitted. The journal serves the interest of both practicing clinicians and researchers.
In addition to original papers, we are launching a range of new manuscript types, including Consensus and Position Papers, Systematic Reviews, Meta-analyses, and Short communications. Case reports are no longer acceptable. Controversial techniques, issues on health policy and social medicine are discussed and serve as useful tools for encouraging debate.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


