倍他受体阻滞剂和维拉帕米对肥厚型心肌病患者心脏预后影响的比较
IF 2.3
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
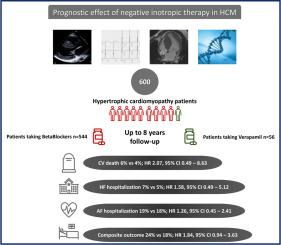
指南建议将倍他受体阻滞剂作为有症状的肥厚型心肌病患者的一线疗法,而将非二氢吡啶类钙通道阻滞剂(尤其是维拉帕米)作为二线疗法,尽管这两种药物之间缺乏对比试验。据报道,维拉帕米在这种情况下会产生有害影响,因此本分析旨在评估肥厚型心肌病患者队列中的受体阻滞剂和维拉帕米对预后的影响。我们从法国肥厚型心肌病前瞻性观察登记处(REMY)收录的全国范围内 1434 名确诊为肥厚型心肌病的患者队列中,回顾性分析了三大中心收录的、接受过倍他受体阻滞剂或维拉帕米治疗的肉芽肿型肥厚型心肌病患者。使用心脏除颤器或心脏起搏器或接受过心房颤动或房间隔消融术的患者不包括在内。主要终点是心血管死亡、心力衰竭住院和心房颤动住院的综合结果。在600名肥厚型心肌病患者中,544人(91%)接受了倍他受体阻滞剂治疗,56人(9%)接受了维拉帕米治疗。在纳入时,两组患者在梗阻存在/程度和心脏性猝死风险因素方面具有可比性。在长达 8 年的随访中(中位数为 3.9 年,IQR 为 2.1-5.8),未观察到主要终点有显著差异(使用倍他受体阻滞剂或维拉帕米的患者分别为 132 [24%] 对 10 [18%],HR=1.84,95% CI=0.94-3.63)。总之,在肥厚型心肌病低风险患者的真实世界队列中,维拉帕米疗法与倍他受体阻滞剂疗法相比,不良事件发生率并不高。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Comparative Influences of Beta blockers and Verapamil on Cardiac Outcomes in Hypertrophic Cardiomyopathy
Guidelines recommend β blockers (BBs) as first-line therapy in symptomatic patients with hypertrophic cardiomyopathy (HCM) and nondihydropyridine calcium channel blockers, particularly, verapamil, as the second-line therapy, despite the absence of comparison trials between those 2 drugs. Because deleterious effects of verapamil have been reported in this setting, the present analysis aimed to evaluate the prognostic impact of BBs and verapamil in a cohort of patients with HCM. From a nationwide cohort of 1,434 patients with a diagnosis of HCM included in the French prospective observational REgistry of hypertrophic cardioMYopathy (REMY), we retrospectively analyzed patients with sarcomeric HCM included in the 3 largest centers and treated either with BBs or verapamil. Patients with a cardiac defibrillator or a pacemaker or who underwent a procedure of atrial fibrillation or septal ablation were excluded. The primary end point was the composite of cardiovascular death, hospitalization for heart failure, and hospitalization for atrial fibrillation. Of 600 patients with HCM, 544 (91%) were treated with BBs and 56 (9%) with verapamil. At inclusion, the 2 groups were comparable concerning the presence/amplitude of obstruction and sudden cardiac death risk factors. At up to 8 years of follow-up (median 3.9 years, interquartile range 2.1 to 5.8), no significant differences were observed in the primary end point (132 [24%] vs 10 [18%] under BBs or verapamil, respectively, hazard ratio 1.84, 95% confidence interval 0.94 to 3.63). In conclusion, in a real-world cohort of low-risk patients with HCM, verapamil therapy was not associated with a higher incidence of adverse events than β-blocker therapy.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

American Journal of Cardiology
医学-心血管系统
CiteScore
4.00
自引率
3.60%
发文量
698
审稿时长
33 days
期刊介绍:
Published 24 times a year, The American Journal of Cardiology® is an independent journal designed for cardiovascular disease specialists and internists with a subspecialty in cardiology throughout the world. AJC is an independent, scientific, peer-reviewed journal of original articles that focus on the practical, clinical approach to the diagnosis and treatment of cardiovascular disease. AJC has one of the fastest acceptance to publication times in Cardiology. Features report on systemic hypertension, methodology, drugs, pacing, arrhythmia, preventive cardiology, congestive heart failure, valvular heart disease, congenital heart disease, and cardiomyopathy. Also included are editorials, readers'' comments, and symposia.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


