心肌梗塞会增加睡眠时间,从而限制心脏炎症和损伤
IF 48.5
1区 综合性期刊
Q1 MULTIDISCIPLINARY SCIENCES
引用次数: 0
摘要
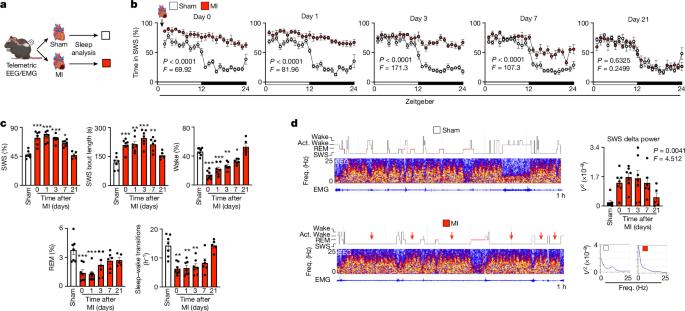
睡眠与心血管健康密不可分1,2。然而,人们对心血管病变与睡眠之间的联系尚未完全了解。目前仍不清楚心脏损伤是否会影响睡眠,以及睡眠介导的神经输出是否有助于心脏愈合和炎症。在这里,我们报告了在人类和小鼠中,心肌梗死(MI)后单核细胞会被积极招募到大脑以促进睡眠,从而抑制心脏的交感神经外流,限制炎症并促进愈合。心肌梗死后,小胶质细胞迅速招募循环中的单核细胞,通过脉络丛进入大脑丘脑外侧后核(LPN),并在那里重新编程生成肿瘤坏死因子(TNF)。在丘脑LPN中,单细胞TNF与表达Tnfrsf1a的谷氨酸能神经元结合,增加慢波睡眠的压力和丰度。心肌梗死后中断睡眠会恶化心脏功能,降低心率变异性,并导致自发性室性心动过速。心肌梗死后,通过操纵丘脑LPN的谷氨酸能TNF信号来扰乱或减少睡眠会增加心脏交感神经的输入,而交感神经通过巨噬细胞的β2-肾上腺素能受体发出信号,促进单核细胞流入的趋化特征。急性冠状动脉综合征后数周内睡眠不足会增加继发性心血管事件的易感性,并降低心脏功能的恢复能力。与此同时,人类睡眠不足会使β2-肾上腺素能受体表达的单核细胞重编程为趋化表型,从而增强其迁移能力。总之,我们的数据揭示了心脏损伤后睡眠的心源性调节,它限制了心脏交感神经的输入,从而限制了炎症和损伤。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Myocardial infarction augments sleep to limit cardiac inflammation and damage
Sleep is integral to cardiovascular health1,2. Yet, the circuits that connect cardiovascular pathology and sleep are incompletely understood. It remains unclear whether cardiac injury influences sleep and whether sleep-mediated neural outputs contribute to heart healing and inflammation. Here we report that in humans and mice, monocytes are actively recruited to the brain after myocardial infarction (MI) to augment sleep, which suppresses sympathetic outflow to the heart, limiting inflammation and promoting healing. After MI, microglia rapidly recruit circulating monocytes to the brain’s thalamic lateral posterior nucleus (LPN) via the choroid plexus, where they are reprogrammed to generate tumour necrosis factor (TNF). In the thalamic LPN, monocytic TNF engages Tnfrsf1a-expressing glutamatergic neurons to increase slow wave sleep pressure and abundance. Disrupting sleep after MI worsens cardiac function, decreases heart rate variability and causes spontaneous ventricular tachycardia. After MI, disrupting or curtailing sleep by manipulating glutamatergic TNF signalling in the thalamic LPN increases cardiac sympathetic input which signals through the β2-adrenergic receptor of macrophages to promote a chemotactic signature that increases monocyte influx. Poor sleep in the weeks following acute coronary syndrome increases susceptibility to secondary cardiovascular events and reduces the heart’s functional recovery. In parallel, insufficient sleep in humans reprogrammes β2-adrenergic receptor-expressing monocytes towards a chemotactic phenotype, enhancing their migratory capacity. Collectively, our data uncover cardiogenic regulation of sleep after heart injury, which restricts cardiac sympathetic input, limiting inflammation and damage. Studies in humans and mice show that myocardial infarction recruits monocytes to the brain’s thalamus, promoting sleep, which in turn restricts cardiac inflammation and sympathetic signalling and assists healing.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Nature
综合性期刊-综合性期刊
CiteScore
90.00
自引率
1.20%
发文量
3652
审稿时长
3 months
期刊介绍:
Nature is a prestigious international journal that publishes peer-reviewed research in various scientific and technological fields. The selection of articles is based on criteria such as originality, importance, interdisciplinary relevance, timeliness, accessibility, elegance, and surprising conclusions. In addition to showcasing significant scientific advances, Nature delivers rapid, authoritative, insightful news, and interpretation of current and upcoming trends impacting science, scientists, and the broader public. The journal serves a dual purpose: firstly, to promptly share noteworthy scientific advances and foster discussions among scientists, and secondly, to ensure the swift dissemination of scientific results globally, emphasizing their significance for knowledge, culture, and daily life.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


