罕见妇科癌症放疗后盆底功能障碍的康复治疗:病例报告
IF 1.2
Q3 OBSTETRICS & GYNECOLOGY
引用次数: 0
摘要
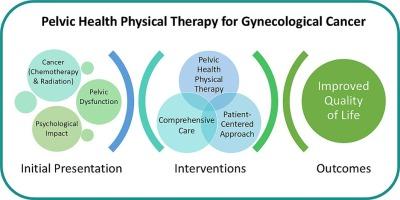
目的:妇科癌症放疗(RT)对患者的性功能障碍、尿失禁(UI)、大便失禁(FI)和心理压力等生活质量有很大影响。有关癌症幸存者盆腔健康物理治疗(PHPT)的包容性治疗方法的文献很少。因此,本病例介绍了一种综合的 PHPT 方案,以解决因 RT 导致的盆底功能障碍的复杂性。病例描述一名 54 岁的女性被诊断为阴道高级别神经内分泌癌。经过为期一年的化疗和 RT 治疗后,患者出现全身乏力、心理困扰、排便困难、混合性尿失禁、便急和排便困难以及双侧外阴淋巴水肿。PHPT 检查显示阴道干涩、外阴阴道纤维化和盆底肌(PFM)无力。PHPT 结合了运动学习、盆底肌的强化和拉伸、盆底肌和外阴组织的内外筋膜活动、淋巴引流、阴道扩张器、疼痛神经科学教育和营养建议。经过七次治疗后,患者的 PFM 强度得到改善,心理社会措施得到改善,无 UI 或 FI,性交时的不适感也有所减轻。然而,考虑到妇科癌症幸存者生理和心理康复所需的持续性和时间,建议继续执行为实现患者目标而制定的护理计划和家庭方案。PHPT疗法包括手法治疗、锻炼、教育和激励性访谈策略,优先考虑患者的目标,并建立了良好的医患关系,迅速取得了最大程度的改善。我们强烈建议医疗服务提供者转介 PHPT,因为干预措施可显著改善患者的生活质量。本病例报告遵循《CARE 指南》(Riley 等,2017 年)。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Rehabilitation of pelvic floor dysfunction after radiation therapy for a rare gynecological cancer: A case report
Objective
Radiation therapy (RT) for gynecological cancers has significant effects on patients’ quality of life regarding sexual dysfunction, urinary incontinence (UI), fecal incontinence (FI), and psychological distress. There is a scarcity in literature for the inclusive therapeutic approaches of pelvic health physical therapy (PHPT) for cancer survivors. Therefore, this case describes a comprehensive PHPT program to address the complexity of pelvic floor dysfunctions due to RT.
Case description
A 54-year-old female was diagnosed with high-grade neuroendocrine carcinoma of the vagina. After a one-year treatment of chemotherapy and RT, the patient presented with overall fatigue, psychological distress, dyspareunia, mixed UI, fecal urgency and FI, and bilateral vulvar lymphedema. The PHPT exam revealed vaginal dryness, vulvovaginal fibrosis, and pelvic floor muscle (PFM) weakness.
A comprehensive treatment approach included referrals to multidisciplinary specialists. PHPT incorporated motor learning, strengthening and stretching of PFM, internal and external fascia mobilization for PFM and vulvar tissues, lymphatic drainage, vaginal dilators, pain neuroscience education and nutrition recommendations. After seven sessions, the patient demonstrated improved PFM strength, improved psychosocial measures, no UI or FI, as well as reduced discomfort during intercourse.
Conclusions
Symptoms were clinically improved with a multidisciplinary approach and comprehensive PHPT. However, considering the consistency and time required for physiological and psychological recovery for gynecological cancer survivors, it was recommended to continue the plan of care and home program developed to address the patient’s goals.
Impact statement
Treatment utilized a holistic and interdisciplinary approach to address the multifactorial nature of vaginal cancer and side effects of RT. PHPT, which promptly maximized improvement, included manual therapy, exercises, education, and motivational interviewing strategies that prioritized the patient’s goals and built a nurturing clinician-patient relationship. Health care providers are strongly encouraged to refer to PHPT as interventions may significantly improve the patient’s quality of life.
This case report follows the CARE Guidelines (Riley et al., 2017).
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Gynecologic Oncology Reports
OBSTETRICS & GYNECOLOGY-
CiteScore
2.00
自引率
0.00%
发文量
183
审稿时长
41 days
期刊介绍:
Gynecologic Oncology Reports is an online-only, open access journal devoted to the rapid publication of narrative review articles, survey articles, case reports, case series, letters to the editor regarding previously published manuscripts and other short communications in the field of gynecologic oncology. The journal will consider papers that concern tumors of the female reproductive tract, with originality, quality, and clarity the chief criteria of acceptance.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


