LUDT-ADHF 试验:针对急性失代偿性心力衰竭住院患者的肺部超声引导下利尿疗法:一项开放标签临床试验。
IF 2.4
4区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
背景 急性失代偿性心力衰竭(ADHF)是入院治疗的主要原因,也是导致发病率和死亡率上升的重要原因。有限的研究表明,肺部超声(LUS)可加强对 ADHF 患者的护理。目的 本研究旨在评估 LUS 引导下的利尿剂治疗对缩短 ADHF 患者住院时间(LOS)和 90 天再入院率的影响。方法 这项开放标签、非随机临床试验纳入了根据 LUS 发现的 B 线和胸腔积液使用利尿剂治疗的 ADHF 患者(LUS 组)与接受标准治疗的患者(对照组)。主要结果是入院时的住院时间,次要结果包括 90 天 ADHF 再入院率、全因再入院率以及急性肾损伤、低钾血症和低血压等安全性参数。结果 研究共纳入 77 名患者,分为两组:对照组和 LUS 组。患者的中位年龄为 68 岁,女性略多于男性(53.25%,n=41)。最常见的合并症是高血压(88.31%,n=68)、糖尿病(59.74%,n=46)和慢性肾病(66.23%,n=51)。LUS 组患者的住院时间较短,但无统计学意义(4 对 5 天,P= 0.175)。与对照组相比,LUS 组患者的 90 天 ADHF 再入院率明显较低(10.53% 对 35.9%;P= 0.175)。本文章由计算机程序翻译,如有差异,请以英文原文为准。
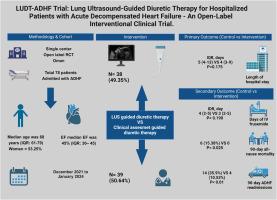
LUDT-ADHF trial: Lung ultrasound-guided diuretic therapy for hospitalized patients with acute decompensated heart failure: An open-label clinical trial
Background Acute Decompensated Heart Failure (ADHF) constitutes a major reason for hospital admissions and significantly contributes to increased morbidity and mortality. Limited research indicates that lung ultrasound (LUS) may enhance the care for patients with ADHF.
Objectives The purpose of this study was to evaluate the impact of LUS-guided diuretic therapy on reducing length of hospital stay (LOS) and 90-day readmissions among patients with ADHF.
Methods This open-label, non-randomized clinical trial included patients with ADHF managed with diuretics based on LUS findings of B-lines and pleural effusion (LUS group) compared to those receiving standard care (control group). The primary outcome was LOS during the index admission, and secondary outcomes included 90-day ADHF readmissions, all-cause readmissions, and safety parameters like acute kidney injury, hypokalemia, and hypotension.
Results The study included a total of 77 patients, segregated into two groups: control and LUS. The median age of the patients was 68 years, with women slightly outnumbering men (53.25%, n=41). The most prevalent comorbidities were hypertension (88.31%, n=68), diabetes mellitus (59.74%, n=46), and chronic kidney disease (66.23%, n=51). The LUS group had a shorter LOS, though not statistically significant (4 vs five days, p= 0.175). Patients in the LUS group had significantly fewer 90-day ADHF readmissions compared to the control group (10.53% vs. 35.9%; p<0.01). Survival analysis demonstrated that the LUS group had a longer time to 90-day ADHF readmissions, with a hazard ratio (HR) of 0.24 (95% CI: 0.08–0.75, p=0.014). For 90-day all-cause readmissions, the LUS group also showed a longer time to readmission compared to controls, with an HR of 0.45 (95% CI: 0.200–1.005, p=0.046). For other safety measures, there was no significant difference in the incidence of adverse events, including acute kidney injury, hypokalaemia, or hypotension, between the LUS and control groups.
Conclusion LUS might reduce in-hospital mortality and readmissions among adults with acute decompensated HF. However, further double-blinded randomized clinical trials are needed to confirm these preliminary results.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Heart & Lung
医学-呼吸系统
CiteScore
4.60
自引率
3.60%
发文量
184
审稿时长
35 days
期刊介绍:
Heart & Lung: The Journal of Cardiopulmonary and Acute Care, the official publication of The American Association of Heart Failure Nurses, presents original, peer-reviewed articles on techniques, advances, investigations, and observations related to the care of patients with acute and critical illness and patients with chronic cardiac or pulmonary disorders.
The Journal''s acute care articles focus on the care of hospitalized patients, including those in the critical and acute care settings. Because most patients who are hospitalized in acute and critical care settings have chronic conditions, we are also interested in the chronically critically ill, the care of patients with chronic cardiopulmonary disorders, their rehabilitation, and disease prevention. The Journal''s heart failure articles focus on all aspects of the care of patients with this condition. Manuscripts that are relevant to populations across the human lifespan are welcome.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


