肠道微生物群介导解郁安神颗粒对2型糖尿病β细胞去分化的缓解作用
IF 8.3
1区 医学
Q1 CHEMISTRY, MEDICINAL
引用次数: 0
摘要
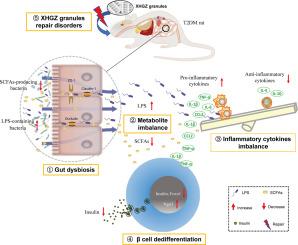
背景:2 型糖尿病(T2DM)是一个全球性的公共健康问题,其特征是 β 细胞功能逐渐衰退。中医理论认为,"上火 "和 "气虚 "是 T2DM 的重要病因,清 "火 "补 "气"(拼音名:Xiehuo-Guzheng,XHGZ)是治疗的重要方法。多年来,我们观察到它对糖尿病的益处。目的:基于肠道微生物群研究 XHGZ 颗粒抗 T2DM β 细胞去分化的机制:方法:通过腹腔注射链脲佐菌素诱导T2DM大鼠食用高脂饮食八周后,随机分配大鼠连续八周服用XHGZ颗粒、二甲双胍或蒸馏水。实验检测了代谢参数、β细胞去分化、炎症细胞因子、肠道微生物群和微生物代谢物(脂多糖(LPS)和短链脂肪酸(SCFAs))的变化。此外,还进行了粪便微生物群移植(FMT),以证实 XHGZ 颗粒调节的肠道微生物群对假性无胚胎 T2DM 大鼠的抗糖尿病作用:结果:XHGZ颗粒能明显改善T2DM大鼠的高血糖症状,改善胰岛功能和病理变化,减少β细胞的去分化和促炎细胞因子。16S rRNA 测序显示,XHGZ 颗粒减少了含 LPS 的微生物群(如 Colidextribacter、Desulfovibrionaceae 和 Morganella),增加了产生 SCFAs 的细菌(如 Prevotella、Alloprevotella 和 Muribaculaceae)和肠道乳杆菌。相应地,它加强了肠道屏障,降低了 LPS,增加了乙酸和丁酸。Tax4Fun分析表明,XHGZ颗粒能恢复异常代谢、脂多糖生物合成以及泛酸和CoA生物合成。此外,XHGZ颗粒调控的微生物群还具有抗糖尿病、抗β细胞脱分化和抗炎的作用,同时减少了假性无胚胎T2DM大鼠体内的LPS,增加了SCFAs:我们的研究结果表明,XHGZ颗粒能通过调节肠道微生物群及其代谢产物缓解T2DM大鼠的β细胞去分化,这表明它有潜力成为T2DM的一种辅助治疗方法。据我们所知,关于中药缓解β细胞去分化的研究还很少,从肠道菌群和微生物代谢产物角度研究其机制的研究也尚未见报道。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Gut microbiota mediate the alleviation effect of Xiehuo-Guzheng granules on β cell dedifferentiation in type 2 diabetes mellitus
Background
Type 2 diabetes mellitus (T2DM) is a worldwide public health problem characterized by a progressive decline in β cell function. In traditional Chinese medicine (TCM) theory, ‘fire’ and ‘healthy qi deficiency’ are important pathogeneses of T2DM, and purging ‘fire’ and reinforcing the ‘healthy qi’ (Pinyin name: Xiehuo-Guzheng, XHGZ) are important method of treatment. Over the years, we have observed its benefit for diabetes. However, the underlying mechanisms remain unclear.
Purpose
To investigate the mechanism of XHGZ granules against β cell dedifferentiation in T2DM based on gut microbiota.
Methods
Rats with T2DM, induced by intraperitoneal injection of streptozotocin after eight weeks of high-fat diet, were randomly allocated to receive XHGZ granules, metformin, or distilled water for eight consecutive weeks. Changes in metabolic parameters, β cell dedifferentiation, inflammatory cytokines, gut microbiota, and microbial metabolites (lipopolysaccharide (LPS) and short-chain fatty acids (SCFAs)), were detected. Furthermore, faecal microbiota transplantation (FMT) was performed to confirm the anti-diabetic effect of XHGZ granule-regulated gut microbiota in pseudo-germ-free T2DM rats.
Results
XHGZ granules significantly ameliorated hyperglycaemia, improved islet function and pathology, and reduced β cell dedifferentiation and pro-inflammatory cytokines in T2DM rats. 16S rRNA sequencing revealed that XHGZ granules decreased the LPS-containing microbiota (e.g., Colidextribacter, Desulfovibrionaceae, and Morganella) and increased the SCFAs-producing bacteria (e.g., Prevotella, Alloprevotella, and Muribaculaceae) and Lactobacillus_intestinalis. Correspondingly, it strengthened intestinal barrier, lowered LPS, and elevated acetic and butyric acids. Tax4Fun analysis indicated that XHGZ granules restored abnormal metabolism, lipopolysaccharide biosynthesis, and pantothenate and CoA biosynthesis. Moreover, the XHGZ granule-regulated microbiota also exhibited the effects of anti-diabetes, anti-β cell dedifferentiation, and anti-inflammation along with the reduction of LPS and the increase of SCFAs in pseudo-germ-free T2DM rats.
Conclusion
Our results show that XHGZ granules alleviate β cell dedifferentiation via regulating gut microbiota and their metabolites in T2DM, suggesting its potential as a promising complementary treatment for T2DM. As far as we know, there are very few studies on the alleviation of β cell dedifferentiation by TCM, and investigations into the mechanism from the perspective of intestinal flora and microbial metabolites are yet to be reported.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Phytomedicine
医学-药学
CiteScore
10.30
自引率
5.10%
发文量
670
审稿时长
91 days
期刊介绍:
Phytomedicine is a therapy-oriented journal that publishes innovative studies on the efficacy, safety, quality, and mechanisms of action of specified plant extracts, phytopharmaceuticals, and their isolated constituents. This includes clinical, pharmacological, pharmacokinetic, and toxicological studies of herbal medicinal products, preparations, and purified compounds with defined and consistent quality, ensuring reproducible pharmacological activity. Founded in 1994, Phytomedicine aims to focus and stimulate research in this field and establish internationally accepted scientific standards for pharmacological studies, proof of clinical efficacy, and safety of phytomedicines.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


