对肥胖进行亚分类,精准预测心脏代谢疾病
IF 50
1区 医学
Q1 BIOCHEMISTRY & MOLECULAR BIOLOGY
引用次数: 0
摘要
肥胖和心脏代谢疾病经常同时发生,但并非总是如此。区分哪些亚人群的心脏代谢风险不同于特定体重指数(BMI)的预期风险,有助于精准预防心脏代谢疾病。因此,我们在四个欧洲人群队列(N ≈ 17.3 万)中进行了无监督聚类。我们发现了五种不一致的特征,其中一些人的心脏代谢生物标志物高于或低于其体重指数(体重指数通常会增加疾病风险)的预期值,总共占总人口的约 20%。在主要不良心血管事件(MACE)和 2 型糖尿病的发病率和未来风险方面,具有不一致特征的人与一致特征的人有所不同。生物标志物中微妙的 BMI 不一致会影响疾病风险。例如,血脂不一致的概率每增加 10%,MACE 风险就会增加 5%(女性的危险比为 1.05,95% 置信区间为 1.03,1.06,P = 4.19 × 10-10;男性的危险比为 1.05,95% 置信区间为 1.04,1.06,P = 9.33 × 10-14)。当纳入不一致的资料信息时,MACE 和 2 型糖尿病的多变量预测模型表现更好(似然比检验 P < 0.001)。这一改进代表着每 10000 名受测者可额外获得 4-15 次正确干预和 37-135 次不必要干预的净收益。本文章由计算机程序翻译,如有差异,请以英文原文为准。

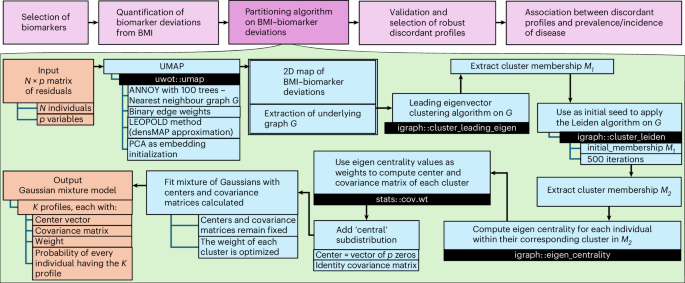
Subclassification of obesity for precision prediction of cardiometabolic diseases
Obesity and cardiometabolic disease often, but not always, coincide. Distinguishing subpopulations within which cardiometabolic risk diverges from the risk expected for a given body mass index (BMI) may facilitate precision prevention of cardiometabolic diseases. Accordingly, we performed unsupervised clustering in four European population-based cohorts (N ≈ 173,000). We detected five discordant profiles consisting of individuals with cardiometabolic biomarkers higher or lower than expected given their BMI, which generally increases disease risk, in total representing ~20% of the total population. Persons with discordant profiles differed from concordant individuals in prevalence and future risk of major adverse cardiovascular events (MACE) and type 2 diabetes. Subtle BMI-discordances in biomarkers affected disease risk. For instance, a 10% higher probability of having a discordant lipid profile was associated with a 5% higher risk of MACE (hazard ratio in women 1.05, 95% confidence interval 1.03, 1.06, P = 4.19 × 10−10; hazard ratio in men 1.05, 95% confidence interval 1.04, 1.06, P = 9.33 × 10−14). Multivariate prediction models for MACE and type 2 diabetes performed better when incorporating discordant profile information (likelihood ratio test P < 0.001). This enhancement represents an additional net benefit of 4−15 additional correct interventions and 37−135 additional unnecessary interventions correctly avoided for every 10,000 individuals tested. A precision medicine approach used unsupervised clustering to identify five distinct phenotypic profiles that can better predict risks of cardiometabolic disease compared with those ascertained based on the additive value of body mass index and other biomarkers, and validated these findings across four independent cohorts.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Nature Medicine
医学-生化与分子生物学
CiteScore
100.90
自引率
0.70%
发文量
525
审稿时长
1 months
期刊介绍:
Nature Medicine is a monthly journal publishing original peer-reviewed research in all areas of medicine. The publication focuses on originality, timeliness, interdisciplinary interest, and the impact on improving human health. In addition to research articles, Nature Medicine also publishes commissioned content such as News, Reviews, and Perspectives. This content aims to provide context for the latest advances in translational and clinical research, reaching a wide audience of M.D. and Ph.D. readers. All editorial decisions for the journal are made by a team of full-time professional editors.
Nature Medicine consider all types of clinical research, including:
-Case-reports and small case series
-Clinical trials, whether phase 1, 2, 3 or 4
-Observational studies
-Meta-analyses
-Biomarker studies
-Public and global health studies
Nature Medicine is also committed to facilitating communication between translational and clinical researchers. As such, we consider “hybrid” studies with preclinical and translational findings reported alongside data from clinical studies.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


