心衰和射血分数降低患者停止长期药物治疗的后果
IF 21.7
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
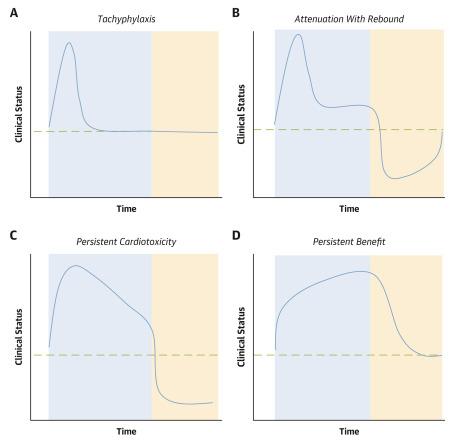
长期服用治疗心力衰竭的药物后,停药的临床效果尚不确定。停用长期治疗药物有 4 种不同的模式:1)治疗效果消失,停药后未观察到任何变化(如哌唑嗪);2)治疗效果减弱或消失,停药后临床恶化反弹(如硝普钠);3) 持续存在有害的治疗效果,停药后临床症状恶化(如米力农和氟氯喹南);以及 4) 持续存在有利的治疗效果,停药后临床症状恶化(如地高辛和钠-葡萄糖共转运体 2 抑制剂)。地高辛、利尿剂、钠-葡萄糖共转运体 2 抑制剂以及(在一定程度上)血管紧张素转换酶抑制剂的疗效持续性已被证明具有说服力。关于停用神经激素拮抗剂后临床状况恶化的现有证据主要包括观察性研究。然而,这些研究结果很难解释,因为停药是出于临床原因,而临床原因比停用有效药物更容易导致这些患者的不良预后。尽管如此,现有的全部证据都表明,大多数用于治疗心力衰竭的药物在停药后几周内都会出现明显的临床恶化。这些研究结果表明,我们目前在强调实施基础药物的同时,还需要同样重视避免出现短期的治疗空白。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Consequences of Discontinuing Long-Term Drug Treatment in Patients With Heart Failure and Reduced Ejection Fraction
There is uncertainty regarding the clinical effects of discontinuation of drugs for heart failure after long-term use. The withdrawal of long-term treatment can follow 1 of 4 distinct patterns: 1) loss of on-treatment effect with no observed changes following discontinuation (eg, prazosin); 2) attenuation or loss of on-treatment effect with rebound clinical worsening following discontinuation (eg, nitroprusside); 3) persistence of deleterious on-treatment effect followed by clinical worsening after discontinuation (eg, milrinone and flosequinan); and 4) persistence of favorable on-treatment effect followed by clinical worsening after discontinuation (eg, digoxin and sodium-glucose cotransporter 2 inhibitors). Persuasive evidence for persistence of efficacy has been demonstrated for the use of digoxin, diuretic agents, sodium-glucose cotransporter 2 inhibitors, and (to a limited extent) for angiotensin-converting enzyme inhibitors. Available evidence for worsening of clinical status following the withdrawal of neurohormonal antagonists largely consists of observational studies. However, their findings are difficult to interpret because of considerable confounding related to the fact that drugs were withdrawn for clinical reasons, which represented a more important contributor to the poor outcome of these patients than the withdrawal of an effective drug. Nevertheless, the totality of available evidence points to a meaningful clinical deterioration within a few weeks following the withdrawal for most drugs that have been evaluated for the treatment of heart failure. These findings suggests that that our current emphasis on the implementation of foundational drugs needs to include an equally important emphasis to avoid even short-term gaps in treatment.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
42.70
自引率
3.30%
发文量
5097
审稿时长
2-4 weeks
期刊介绍:
The Journal of the American College of Cardiology (JACC) publishes peer-reviewed articles highlighting all aspects of cardiovascular disease, including original clinical studies, experimental investigations with clear clinical relevance, state-of-the-art papers and viewpoints.
Content Profile:
-Original Investigations
-JACC State-of-the-Art Reviews
-JACC Review Topics of the Week
-Guidelines & Clinical Documents
-JACC Guideline Comparisons
-JACC Scientific Expert Panels
-Cardiovascular Medicine & Society
-Editorial Comments (accompanying every Original Investigation)
-Research Letters
-Fellows-in-Training/Early Career Professional Pages
-Editor’s Pages from the Editor-in-Chief or other invited thought leaders

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


