射血分数降低的肾移植受者的心衰用药和随访模式:单中心经验
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
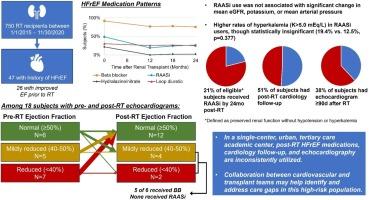
背景对接受肾移植(RT)的终末期肾病患者射血分数降低型心衰(HFrEF)的药物治疗作用研究不足。方法纳入 2015 年 1 月 1 日至 2020 年 11 月 30 日期间接受肾移植且接受肾移植前射血分数(EF)为 40% 的患者。结果和结论47/750(6.3%)例RT受术者之前已确诊为HFrEF,其中26例在RT前EF有所改善。43 名受试者(92%)在 RT 前接受了β受体阻滞剂(BB)治疗,23 名受试者(49%)接受了肾素-血管紧张素-醛固酮抑制剂(RAASi)治疗。手术后 24 个月内,34 名受试者(76%)使用了β受体阻滞剂,12 名受试者(27%)使用了 RAASi。在该队列中,RT 后心脏病学随访率(51%)和超声心动图检查率(38%)低于预期。在 29 名因肾功能保留且随访期间未出现高钾血症或低血压而有可能接受 RAASi 治疗的受试者中,只有 6 人(21%)接受了 RAASi 治疗。在6名RT后EF为50%的受试者中,有4人符合条件,但没有接受RAASi治疗。心脏科和移植团队之间的多学科合作可能有助于改善对这一高风险患者群体的护理。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Heart failure medication use and follow-up patterns in renal transplant recipients with reduced ejection fraction: A single-center experience
Background
The role of medical therapy for heart failure with reduced ejection fraction (HFrEF) in subjects with end-stage renal disease receiving renal transplantation (RT) is understudied. Here, we describe post-RT HFrEF medical management practices at a single urban, academic tertiary care center.
Methods
RT recipients between January 1, 2015 and November 30, 2020 with history of ejection fraction (EF) <40 % prior to RT were included. Medications, renal function, blood pressure, cardiology follow-up, and echocardiograms ≥90d post-RT were retrospectively collected for 2 years post-RT.
Results and conclusions
47/750 (6.3 %) of RT recipients had prior HFrEF diagnosis, of whom 26 experienced improvement in EF prior to RT. Pre-RT medical therapy included beta blocker (BB) in 43 (92 %) of subjects and renin-angiotensin-aldosterone inhibitors (RAASi) in 23 (49 %). By 24 months post-RT, BB were used in 34 (76 %) and RAASi were used in 12 (27 %) of subjects. Rates of post-RT cardiology follow-up (51 %) and echocardiogram (38 %) were lower than expected in this cohort. Of 29 subjects potentially eligible for RAASi based on preserved renal function and no hyperkalemia or hypotension episodes during follow-up, only 6 (21 %) received RAASi. Of 6 subjects with post-RT EF <50 %, 4 were eligible but did not receive RAASi. Multidisciplinary collaboration between cardiology and transplant teams may help improve care for this high-risk patient population.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
IJC Heart and Vasculature
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
4.90
自引率
10.30%
发文量
216
审稿时长
56 days
期刊介绍:
IJC Heart & Vasculature is an online-only, open-access journal dedicated to publishing original articles and reviews (also Editorials and Letters to the Editor) which report on structural and functional cardiovascular pathology, with an emphasis on imaging and disease pathophysiology. Articles must be authentic, educational, clinically relevant, and original in their content and scientific approach. IJC Heart & Vasculature requires the highest standards of scientific integrity in order to promote reliable, reproducible and verifiable research findings. All authors are advised to consult the Principles of Ethical Publishing in the International Journal of Cardiology before submitting a manuscript. Submission of a manuscript to this journal gives the publisher the right to publish that paper if it is accepted. Manuscripts may be edited to improve clarity and expression.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


