秋水仙碱对心肌梗死的影响:随机对照试验的最新系统回顾和元分析》。
IF 3.3
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
导言:心肌梗塞(MI)与严重的事后炎症反应有关,而炎症反应也会影响心肌梗塞后的预后。秋水仙碱是一种抗炎药物,对冠心病、心包炎和心房颤动等各种心血管疾病有潜在疗效。这项荟萃分析的主要目的是对秋水仙碱减少急性心肌梗死患者不良心血管事件的有效性和安全性进行最新评估:在PubMed、Cochrane Library、Scopus、Google Scholar和clinicaltrials.gov上对2024年5月之前研究秋水仙碱对心肌梗死患者影响的随机对照试验(RCT)进行了系统全面的检索。我们的主要研究结果是心血管不良事件的综合结果,次要结果包括全因死亡率、中风发生率、心脏骤停、紧急住院、胃肠道不良事件和高敏C反应蛋白(Hs-CRP)水平。在随机效应模型下对风险比(RR)和标准化平均差(SMD)进行了汇总:共有 11 项试验,7161 名患者参与了分析,其中 3546 人(49.51%)被分配使用秋水仙碱,3591 人(50.14%)使用安慰剂。秋水仙碱对心血管不良事件(RR=0.75,95% CI:0.60-0.94,P=0.01,I2=48%)、急迫住院(RR=0.46,95% CI:0.31-0.68,P=0.0001,I2=0%)和Hs-CRP水平(SMD=-0.43,95% CI:-0.83-0.03,P=0.03,I2=85%),但胃肠道不良事件(RR=1.86,95% CI:1.14-3.02,P=0.01,I2=79%)有统计学意义的显著增加。然而,全因死亡率(RR=1.00,95% CI:0.72-1.39,P=0.98,I2=0%)、心脏骤停(RR=0.81,95% CI:0.33-1.95,P=0.63,I2=0)、中风发生率(RR=0.45,95% CI:0.17-1.19,P=0.11,I2=36%)和复发性心肌梗死(RR=0.78,95% CI:0.57-1.06,P=0.11,I2=11%)在两组中仍具有可比性:结论:心肌梗死后使用秋水仙碱可减少心血管不良事件、Hs-CRP水平、住院急迫性等综合因素,但会增加胃肠道不良事件。不过,秋水仙碱不会影响全因死亡率、心脏骤停、中风发生率和复发性心肌梗死发生率。有必要进行大规模多中心 RCT 研究,尤其是延长随访时间,以验证这些研究结果。本文章由计算机程序翻译,如有差异,请以英文原文为准。
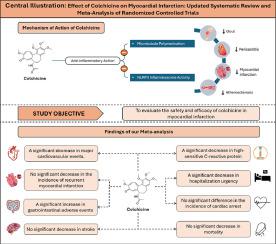
The effect of colchicine on myocardial infarction: An updated systematic review and meta-analysis of randomized controlled trials
Introduction
Myocardial infarction (MI) is associated with a significant post-event inflammatory response which further contributes to post-MI prognosis. Colchicine, an anti-inflammatory agent, exhibits potential benefits in various cardiovascular conditions such as coronary artery disease, pericarditis and atrial fibrillation. This meta-analysis predominantly aimed to provide an up-to-date evaluation of the efficacy and safety of colchicine in reducing adverse cardiovascular events in patients following acute MI.
Methods
A Comprehensive search was conducted on PubMed, Cochrane Library, Scopus, Google Scholar and clinicaltrials.gov for randomized controlled trials (RCTs) investigating the effect of colchicine on patients with MI from inception till May 2024. Our primary outcome was a composite of adverse cardiovascular events, while secondary outcomes included all-cause mortality, incidence of stroke, incidence of cardiac arrest, hospitalization urgency, incidence of recurrent MI, adverse gastrointestinal events and levels of high-sensitivity C - reactive protein (Hs-CRP). Risk ratios (RR) and mean differences (MD) were pooled under the random-effects model.
Results
Eleven trials with 7161 patients were included in our analysis out of which 3546 (49.51 %) were allocated to colchicine and 3591 (50.14 %) received placebo. Colchicine demonstrated statistically significant reduction in the composite of adverse cardiovascular events (RR = 0.75, 95 % CI: 0.60-0.94, P = 0.01, I2 = 47 %), and hospitalization urgency (RR = 0.46, 95 % CI: 0.31-0.68, P = 0.0001, I2 = 0 %) but statistically significant increment in adverse gastrointestinal events (RR = 1.86, 95 % CI: 1.14-3.02, P = 0.01, I2 = 79 %). However, all-cause mortality (RR = 1.00, 95 % CI: 0.72-1.39, P = 0.98, I2 = 0 %), incidence of cardiac arrest (RR = 0.81, 95 % CI: 0.33-1.95, P = 0.63, I2 = 0), incidence of stroke (RR = 0.45, 95 % CI: 0.17-1.19, P = 0.11, I2 = 36 %), incidence of recurrent MI (RR = 0.78, 95 % CI: 0.57-1.06, P = 0.11, I2 = 11 %) and the levels of hs-CRP (MD= -0.87, 95 %CI: -1.80-0.06, P=0.07, I2=67 % remained comparable across the two groups.
Conclusion
The use of colchicine post-MI reduces the composite of adverse cardiovascular events, and hospitalization urgency but increases adverse gastrointestinal events. However, colchicine does not impact all-cause mortality, cardiac arrest, stroke incidence, incidence of recurrent MI and the levels of hs-CRP. Large scale multicenter RCTs especially with longer follow-up duration are warranted to validate these findings.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Current Problems in Cardiology
医学-心血管系统
CiteScore
4.80
自引率
2.40%
发文量
392
审稿时长
6 days
期刊介绍:
Under the editorial leadership of noted cardiologist Dr. Hector O. Ventura, Current Problems in Cardiology provides focused, comprehensive coverage of important clinical topics in cardiology. Each monthly issues, addresses a selected clinical problem or condition, including pathophysiology, invasive and noninvasive diagnosis, drug therapy, surgical management, and rehabilitation; or explores the clinical applications of a diagnostic modality or a particular category of drugs. Critical commentary from the distinguished editorial board accompanies each monograph, providing readers with additional insights. An extensive bibliography in each issue saves hours of library research.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


