胡桃夹子综合症(德尔菲共识)。
IF 2.8
2区 医学
Q2 PERIPHERAL VASCULAR DISEASE
Journal of vascular surgery. Venous and lymphatic disorders
Pub Date : 2025-01-01
DOI:10.1016/j.jvsv.2024.101970
引用次数: 0
摘要
简介胡桃钳综合征是指主动脉和肠系膜上动脉之间的左肾静脉受到无症状的压迫。无症状压迫是一种常见的影像学发现,而胡桃钳综合征患者可报告一系列症状。目前还没有具体的诊断标准,干预措施包括一系列开放手术和血管内手术。因此,我们希望制定一份国际共识文件,涵盖裂颅综合征患者的诊断、管理和随访等方面:方法:我们进行了三阶段改良德尔菲共识。一个指导委员会为胡桃夹综合征患者制定了 37 项声明,涵盖三个类别:诊断、管理和随访。这些声明由 20 位静脉疾病管理方面的国际专家采用五点李克特量表逐一报告。如果≥70%的受访者对声明的评分在1或2分(同意)和4或5分(不同意)之间,则定义为达成共识。未达成一致意见的声明将在第二轮投票中重新传阅。第三轮问卷调查增加了 14 项陈述,以明确胡桃夹综合征的诊断价值:第一轮 20 位专家中有 20 位(100%)做出了答复,第二轮 20 位专家中有 17 位(85%)做出了答复。在所有类别的 37 项陈述中,有 24 项(65%)达成了初步共识。第二轮又就 10 项陈述中的 5 项(50%)达成了共识。没有任何类别就所有陈述达成共识。在第二轮中,就后续行动类别达成了共识(4/5 项声明,80%)。最后一轮就 14 项声明中的 5 项(36%)达成了共识。专家们一致认为影像学检查有义务确认 NCS。专家们并未就具体的诊断临界值达成一致。专家们一致认为手术治疗的首选是左肾静脉转位,支架移位的风险大于经皮手术的优势:结论:关于胡桃夹综合征的评估和治疗,大多数意见已达成共识。德尔菲共识确定了需要进一步研究的领域,如抗血小板治疗、血管内治疗和肾脏自体移植。有必要建立罕见疾病登记册,以改进数据和患者预后报告。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Nutcracker syndrome (a Delphi consensus)
Background
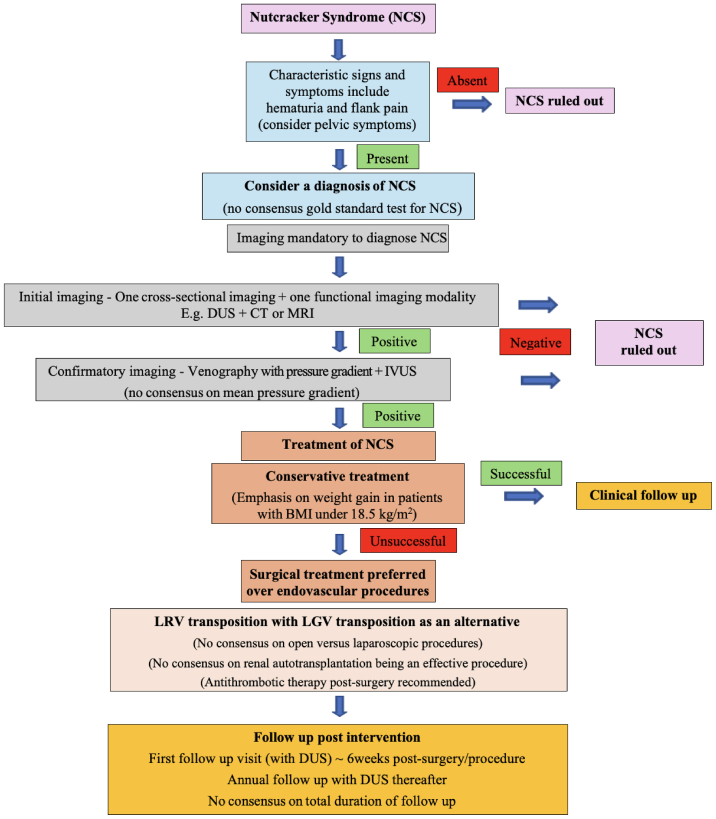
Nutcracker syndrome (NCS) describes the symptomatic compression of the left renal vein between the aorta and superior mesenteric artery. Whereas asymptomatic compression is a common radiological finding, patients with NCS can report a range of symptoms. There are no specific diagnostic criteria and interventions include a range of open surgical and endovascular procedures. Therefore, we wished to develop an international consensus document covering aspects of diagnosis, management, and follow-up for patients with NCS.
Methods
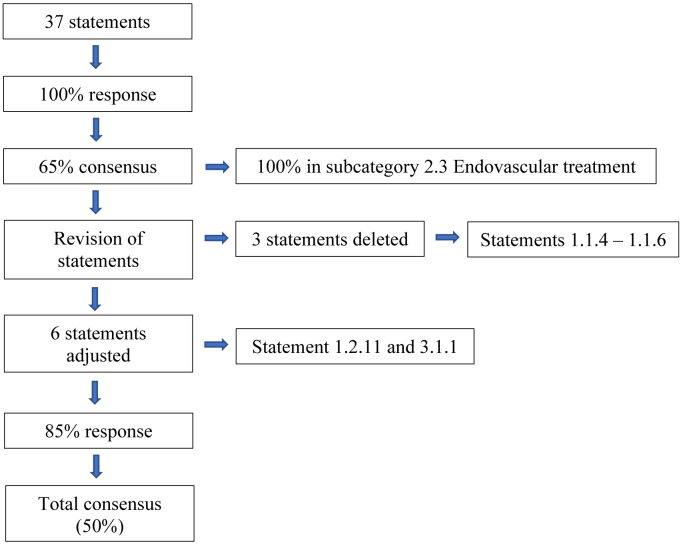
A three-stage modified Delphi consensus was performed. A steering committee developed 37 statements covering 3 categories for patients with NCS: diagnosis, management, and follow-up. These statements were reported individually by 20 international experts in the management of venous disease, using a 5-point Likert scale. Consensus was defined if ≥70% of respondents rated the statement between 1 and 2 (agreement) and between 4 and 5 (disagreement). Those statements without consensus were recirculated in a second round of voting. A third round of the questionnaire was performed with 14 additional statements to clarify diagnostic values of NCS.
Results
Responses were returned by 20 of 20 experts (100%) in round one and 17 of 20 (85%) in round two. Initial consensus was reached in 24 of 37 statements (65%) spread over all categories. Round two achieved a further consensus on 5 out of 10 statements (50%). No categories reported consensus on all statements. In round two consensus was reached in the category of follow-up (4/5 statements [80%]). The final round reached consensus on 5 out of 14 statements (36%). Experts agreed that imaging is obligated to confirm NCS. Experts did not agree on specific diagnostic cut-off values. There was a consensus that the first choice of operative treatment is left renal vein transposition and that the risk of stent migration outweighs the advantages of a percutaneous procedure.
Conclusions
Consensus was achieved on most statements concerning the assessment and management of NCS. This Delphi consensus identified those areas in which further research is needed, such as antiplatelet therapy, endovascular treatment, and renal autotransplantation. A rare disease registry to improve data and reports of patient outcomes is warranted.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of vascular surgery. Venous and lymphatic disorders
SURGERYPERIPHERAL VASCULAR DISEASE&n-PERIPHERAL VASCULAR DISEASE
CiteScore
6.30
自引率
18.80%
发文量
328
审稿时长
71 days
期刊介绍:
Journal of Vascular Surgery: Venous and Lymphatic Disorders is one of a series of specialist journals launched by the Journal of Vascular Surgery. It aims to be the premier international Journal of medical, endovascular and surgical management of venous and lymphatic disorders. It publishes high quality clinical, research, case reports, techniques, and practice manuscripts related to all aspects of venous and lymphatic disorders, including malformations and wound care, with an emphasis on the practicing clinician. The journal seeks to provide novel and timely information to vascular surgeons, interventionalists, phlebologists, wound care specialists, and allied health professionals who treat patients presenting with vascular and lymphatic disorders. As the official publication of The Society for Vascular Surgery and the American Venous Forum, the Journal will publish, after peer review, selected papers presented at the annual meeting of these organizations and affiliated vascular societies, as well as original articles from members and non-members.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


