在一个真实世界的队列中,血浆置换并不能改善急性肝衰竭患者的总生存率
IF 26.8
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
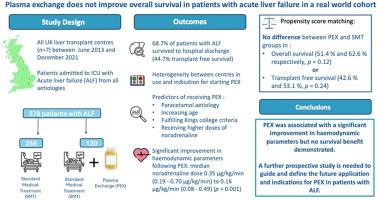
背景和目的治疗性血浆置换(PEX)已成为急性肝衰竭(ALF)患者的一种潜在治疗选择。在临床试验之外,治疗性血浆置换对生存结果的影响尚未得到充分证实。这项多中心回顾性队列研究纳入了 2013 年 6 月至 2021 年 12 月期间入住英国 7 家三级肝移植中心的连续 ALF 患者。研究人员评估了PEX治疗后临床变量的变化,并将接受PEX治疗的患者与接受标准药物治疗(SMT)的患者出院后的总生存率和无移植生存率(TFS)进行了比较。结果我们纳入了378例ALF患者(中位数(IQR)年龄36(28-48)岁,64%(n=242)为女性),其中120例接受了PEX治疗。PEX 后,大多数临床变量都有明显改善,包括去甲肾上腺素的中位剂量(从 0.35 μg/kg/min (0.19 - 0.70 μg/kg/min) 降至 0.16 μg/kg/min (0.08 - 0.49) (p = 0.001)。PEX组和SMT组在总生存率(分别为51.4%对62.6%,p = 0.12)或TFS(42.6%对53.1%,p = 0.24)方面没有明显差异。PEX可明显改善血流动力学参数,但对生存没有益处。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Plasma exchange does not improve overall survival in patients with acute liver failure in a real-world cohort
Background & Aims
Therapeutic plasma exchange (PEX) has emerged as a potential treatment option for patients with acute liver failure (ALF). The effect of PEX on survival outcomes outside of clinical trials is not yet well established. In this study we aimed to evaluate the real-world use and outcomes of PEX for the treatment of ALF.
Methods
This multicentre retrospective cohort study included consecutive patients with ALF admitted to all seven tertiary liver transplant centres in the UK between June 2013 and December 2021. Changes in clinical variables following PEX treatment were assessed, while overall survival and transplant-free survival up to hospital discharge in patients receiving PEX were compared to those receiving standard medical therapy Propensity score matching was performed to control for intergroup covariates and selection bias.
Results
We included 378 patients with ALF (median [IQR] age 36 (28-48), 64% [n = 242] female) of whom 120 received PEX. There was a significant improvement in most clinical variables following PEX, including median dose of noradrenaline (reduction from 0.35 μg/kg/min [0.19–0.70 μg/kg/min] to 0.16 μg/kg/min [0.08–0.49], p = 0.001). There was no significant difference between PEX and standard medical therapy groups in overall survival (51.4% vs. 62.6%, respectively, p = 0.12) or transplant-free survival (42.6% vs. 53.1%, p = 0.24).
Conclusion
PEX is now frequently used in the management of patients with ALF in the UK. It is associated with significant improvement in haemodynamic parameters but not survival benefit.
Impact and implications:
Therapeutic plasma exchange is frequently used in the management of patients with acute liver failure in the UK. This real-world study demonstrates significant improvement in haemodynamic status but has not confirmed the survival benefit seen in previous published literature. These results should help guide the future use of plasma exchange in this patient population.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Hepatology
医学-胃肠肝病学
CiteScore
46.10
自引率
4.30%
发文量
2325
审稿时长
30 days
期刊介绍:
The Journal of Hepatology is the official publication of the European Association for the Study of the Liver (EASL). It is dedicated to presenting clinical and basic research in the field of hepatology through original papers, reviews, case reports, and letters to the Editor. The Journal is published in English and may consider supplements that pass an editorial review.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


