吸烟对急性心肌梗死术后结果和全因死亡率的影响:误导早期假性心肌梗死,最终降低存活率
IF 1.9
Q3 PERIPHERAL VASCULAR DISEASE
International Journal of Cardiology Cardiovascular Risk and Prevention
Pub Date : 2024-09-27
DOI:10.1016/j.ijcrp.2024.200336
引用次数: 0
摘要
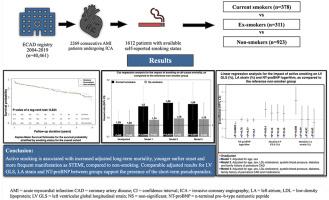
背景吸烟对急性心肌梗死(AMI)后的预后有着相互矛盾的结果。我们评估了吸烟状况对患者预后的独立影响。方法我们纳入了接受有创冠状动脉造影术并能自我报告吸烟状况的急性心肌梗死患者。在中位 1.14 年(0.36-3.40 年)的随访期间,我们评估了各种原因导致的死亡发生率。结果在 1612 名 AMI 患者(年龄为 65.7 ± 13.3 岁,72.1% 为男性)中,有 378 名患者(23.4%)目前吸烟,311 名患者(19.3%)曾经吸烟,923 名患者(57.3%)不吸烟。与非吸烟者相比,当前吸烟者更年轻(68.5 ± 13.0 vs. 58.6 ± 12.5,p < 0.0001),更经常出现 STEMI(21.6 % vs. 35.4 %,p < 0.0001),而曾经吸烟者的 STEMI 发生率与非吸烟者相似(22.5 %,p = 0.79),在年龄上属于中间组(65.8 ± 11.6 岁)。虽然在未经调整的分析中,吸烟状况与长期生存率并无明显关联,但在对年龄、性别、药物和其他传统风险因素进行调整后,主动吸烟者的长期死亡率比不吸烟者高出 56%,而戒烟者的生存概率与主动吸烟者相当(当前吸烟者:1.56[1.14-2.00]):1.56[1.14-2.14],p = 0.006;戒烟者 1.16[0.84-1.59],p = 0.37)。目前吸烟者未经调整的NT-proBNP值较低,院内左心室整体纵向应变(LV GLS)绝对值略高,经同样调整后,各组间无差异(NT-proBNP:-0.08[-0.31; 0.15],p = 0.5,LV GLS:0.65[-0.26; 1.55],p = 0.16)。各组间 LV GLS 和 NT-proBNP 的调整结果相当,这支持了假性动脉粥样硬化的存在。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Impact of smoking on procedural outcomes and all-cause mortality following acute myocardial infarction: A misleading early-stage pseudoparadox with ultimately reduced survival
Background
Smoking has conflicting results on outcomes following acute myocardial infarction (AMI). We evaluated the independent influence of smoking status on patient outcomes.
Methods
We included patients with AMI undergoing invasive coronary angiography with available self-reported smoking status. The incidence of death of any cause was evaluated during a median follow-up of 1.14 years (range 0.36–3.40 years). Association between smoking status and long-term mortality was evaluated using multivariable adjusted Cox regression analysis.
Results
From 1612 AMI patients (aged 65.7 ± 13.3 years, 72.1 % male), 378 patients (23.4 %) were current-smokers, 311 (19.3 %) ex-smokers, and 923 (57.3 %) non-smokers. Compared with non-smokers, current-smokers were younger (68.5 ± 13.0 vs. 58.6 ± 12.5, p < 0.0001) and more frequently presented with STEMI (21.6 % vs. 35,4 %, p < 0.0001), while ex-smokers with similar frequency of STEMI-manifestation as non-smokers (22.5 %, p = 0.79) constituted an intermediate-group in terms of age (65.8 ± 11,6 years). Although smoking status was not significantly associated with long-term survival in unadjusted-analysis, active-smokers had 56 % higher long-term mortality than non-smokers when adjusting for age, gender, medications and other traditional risk factors, whereas ex-smokers possessed comparable survival probability (current-smokers: 1.56[1.14–2.14], p = 0.006, ex-smokers 1.16[0.84–1.59], p = 0.37). Current-smokers had unadjusted lower NT-proBNP and modestly higher absolute in-hospital left ventricular global longitudinal strain (LV GLS) values that did not differ among groups after the same adjustments (NT-proBNP: −0.08[-0.31; 0.15], p = 0.5, LV GLS: 0.65[-0.26; 1.55], p = 0.16).
Conclusion
Active smoking is associated with increased adjusted long-term mortality, earlier onset and more frequent manifestation as STEMI, compared to non-smoking. Comparable adjusted results for LV GLS and NT-proBNP between groups support the presence of the pseudoparadox.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

International Journal of Cardiology Cardiovascular Risk and Prevention
Cardiology and Cardiovascular Medicine
CiteScore
3.00
自引率
0.00%
发文量
0
审稿时长
72 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


