探索个人、家庭和项目特征与加入加拿大儿科体重管理注册机构(CANPWR)12 个月后健康结果变化之间的关系
IF 4.2
2区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
摘要
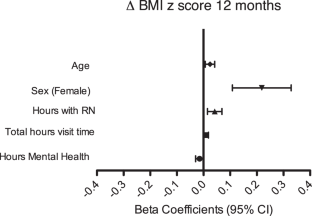
目标研究超重或肥胖儿童在参与多学科肥胖管理 12 个月后,其个人、家庭和项目特征与人体测量和心脏代谢健康指标变化的相关性。方法参与者包括加入加拿大儿科体重管理登记处(CANPWR)的 2-17 岁超重或肥胖儿童。通过多元线性回归分析,研究个人、家庭和项目特征与人体测量(WHO BMI z-score)和心脏代谢健康指标(收缩压和舒张压;口服葡萄糖耐量试验(OGTT)后空腹血糖和2小时血糖;高密度脂蛋白(HDL)和非高密度脂蛋白胆固醇以及空腹甘油三酯)变化之间的关系。结果 基线后 6 个月有 1065/1286 人(82.8%)提供了体重指数 z 值数据,基线后 12 个月有 893/1286 人(69.4%)提供了体重指数 z 值数据。6个月时,BMI z-score相对于基线有所下降(平均差 (MD) [95% 置信区间 (CI)] = -0.08 [-0.10 to -0.06]; p < 0.001)。体重指数 z 值(MD [95% CI] = -0.08 [-0.13 to -0.04);p = 0.001)和空腹甘油三酯(MD [95% CI] = -0.07 [-0.13 to -0.02);p = 0.011)在 12 个月时比基线值有所下降。基线年龄较大(估计值 β = 0.025;95% CI [0.006,0.042],p = 0.007)和女性(估计值 β = 0.241;95% CI [0.108,0.329],p < 0.001)与 12 个月时Δ BMI z 分数的恶化有关,而与心理健康提供者接触的总时数(估计 β = -0.015;95% CI [-0.030,-0.001],p = 0.049)与 12 个月时Δ BMI z 分数的改善有关。与运动顾问接触的时间(估计β = 0.023;95% CI [0.008,0.039],p = 0.003)与高密度脂蛋白的改善有关,而与注册营养师接触的时间(估计β = -0.026;95% CI [-0.051,-0.001],p = 0.044)与非高密度脂蛋白胆固醇的改善有关。结论在基线后的 12 个月中,男性性别以及与心理健康提供者、运动顾问和注册营养师共度的时间与多项人体测量和心脏代谢健康指标的显著改善有关。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Exploring the association between individual, family, and program characteristics and change in health outcomes 12 months after enrollment into the CANadian Pediatric Weight management Registry (CANPWR)
To examine individual, family, and program characteristics associated with changes in anthropometric and cardiometabolic health indicators in children with overweight or obesity after participating in multidisciplinary obesity management for 12 months. Participants included children 2–17 years old with overweight or obesity enrolled in the CANadian Pediatric Weight Management Registry (CANPWR). Multiple linear regression analyses were conducted to investigate the associations between individual, family, and program characteristics and changes in anthropometry (WHO BMI z-score) and cardiometabolic health indicators (systolic and diastolic blood pressure; fasting and 2-h glucose post-oral glucose tolerance test (OGTT); high density lipoprotein- (HDL) and non-HDL cholesterol and fasting triglycerides). BMI z-score data were available from 1065/1286 (82.8%) at 6-months post-baseline and 893/1286 (69.4%) at 12-months post-baseline. At 6-months, BMI z-score decreased relative to baseline (mean difference (MD) [95% confidence interval (CI)] = −0.08 [−0.10 to −0.06]; p < 0.001). BMI z-score (MD [95% CI] = −0.08 [−0.13 to −0.04); p = 0.001) and fasting triglycerides (MD [95% CI] = −0.07 [−0.13 to −0.02); p = 0.011) decreased at 12 months from baseline. Older age at baseline (estimated β = 0.025; 95% CI [0.006, 0.042], p = 0.007) and female sex (estimated β = 0.241; 95% CI [0.108, 0.329], p < 0.001) were associated with a worsened Δ BMI z-score at 12 months, while total hours with mental health provider (estimated β = −0.015; 95% CI [−0.030, −0.001], p = 0.049) was associated with an improved Δ BMI z-score at 12 months. Hours with an exercise counselor (estimated β = 0.023; 95% CI [0.008, 0.039], p = 0.003) were associated with improved HDL, while hours with a registered dietitian (estimated β = −0.026; 95% CI [−0.051, −0.001], p = 0.044) were associated with improved non-HDL cholesterol. Male sex and hours spent with a mental health provider, exercise counselor, and registered dietitian were related to significant improvements in several anthropometric and cardiometabolic health indicators at 12 months post-baseline.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

International Journal of Obesity
医学-内分泌学与代谢
CiteScore
10.00
自引率
2.00%
发文量
221
审稿时长
3 months
期刊介绍:
The International Journal of Obesity is a multi-disciplinary forum for research describing basic, clinical and applied studies in biochemistry, physiology, genetics and nutrition, molecular, metabolic, psychological and epidemiological aspects of obesity and related disorders.
We publish a range of content types including original research articles, technical reports, reviews, correspondence and brief communications that elaborate on significant advances in the field and cover topical issues.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


