减肥手术后的酒精使用障碍:一项使用关联健康索赔和调查数据进行的研究。
IF 3.8
2区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
摘要
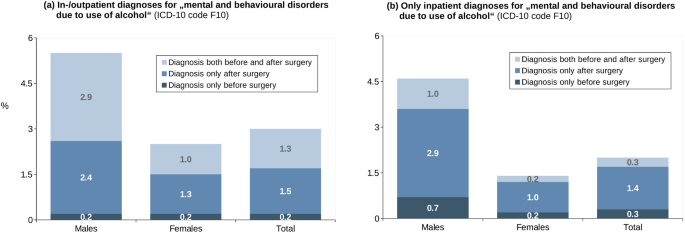
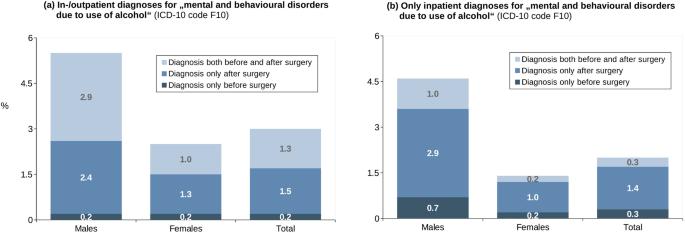
背景:以前的研究曾多次报告过减肥手术(BS)后患者的酒精使用障碍(AUDs)。将健康索赔数据与调查数据相结合的研究将使这一研究领域受益匪浅:基于一项回顾性队列研究和横断面研究,我们对大型健康索赔数据库中的 2151 名减肥手术患者进行了问卷调查,根据有效工具(AUDIT)和健康索赔数据中的 ICD-10 编码评估了患者是否存在 AUDs。我们从性别、手术后时间、对减肥的满意度和医疗资源利用率(HCRU)等方面对有和无 AUDs 的患者进行了描述:大多数患者为女性(80.7%),手术后的中位时间为 6 年(四分位距:4-9 年)。大多数患者的减肥手术是 RYGB-旁路术(50%)或袖状胃切除术(43%)。总体而言,3% 的患者在索赔数据中至少有一个 AUD 诊断代码(男性:5.5%,女性:2.5%)。在男性中,43.6% 的诊断代码是在手术后而非手术前输入的(女性:52%)。根据 AUDIT(由 1496 名患者填写),9.4% 的患者至少有危险/有害饮酒行为。得分较高与患者性别、手术后时间较长、对体重减轻不满意以及HCRU较高有关,而心理治疗方面的结果则相互矛盾:结论:研究人群中的酒精成瘾者比例令人担忧,因为 BS 术后应限制饮酒。研究结果表明,有必要对患者进行密切监测和术后护理。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Alcohol use disorders after bariatric surgery: a study using linked health claims and survey data
Previous studies have repeatedly reported alcohol use disorders (AUDs) in patients after bariatric surgery (BS). This research field can benefit from studies combining health claims data with survey data. Based on a combined retrospective cohort and cross-sectional study, 2151 patients with BS identified in a large health claims database received a questionnaire, by which we assessed the presence of AUDs based on a validated instrument (AUDIT) as well as by ICD-10 codes from the health claims data. We described patients with vs. without AUDs regarding sex, time since surgery, satisfaction with weight loss and health care resource utilization (HCRU). The majority of patients were female (80.7%) with a median time since surgery of 6 years (Interquartile range: 4–9 years). For the majority of patients, the bariatric intervention was either a RYGB-Bypass (50%) or sleeve gastrectomy (43%). Overall, 3% had at least one AUD diagnosis code in the claims data (men: 5.5%, women: 2.5%). Among men, 43.6% of diagnoses were coded after but not before the surgery (women: 52%). According to AUDIT (completed by 1496 patients), 9.4% of all patients showed at least hazardous/harmful alcohol consumption. Higher scores were associated with sex of the person, longer time since surgery, dissatisfaction with the weight loss and higher HCRU, with contradicting results regarding psychotherapeutic care. The proportion with AUDs in the study population gives rise to concern as alcohol consumption should be restricted after BS. The results suggest the necessity for close monitoring and post-surgical care.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

International Journal of Obesity
医学-内分泌学与代谢
CiteScore
10.00
自引率
2.00%
发文量
221
审稿时长
3 months
期刊介绍:
The International Journal of Obesity is a multi-disciplinary forum for research describing basic, clinical and applied studies in biochemistry, physiology, genetics and nutrition, molecular, metabolic, psychological and epidemiological aspects of obesity and related disorders.
We publish a range of content types including original research articles, technical reports, reviews, correspondence and brief communications that elaborate on significant advances in the field and cover topical issues.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


