胰腺癌切除术后的快速转移性复发:二十年来手术失败趋势的多中心区域分析。
IF 2.7
3区 医学
Q2 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
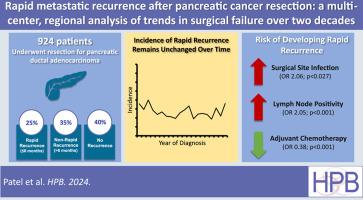
背景:胰腺导管腺癌(PDAc)是一种致命的恶性肿瘤,部分原因是切除术后的快速复发率(rrPDAc)很高。我们试图描述随着时间推移的复发率,并研究预测rrPDAc的因素:方法:我们查询了一个地区性多机构癌症登记处,并从国家手术质量改进计划数据库中获取数据,以了解 1996 年至 2020 年期间 PDAc 患者的情况。RrPDAc 被定义为治愈性切除术后 6 个月内的复发:我们确定了 924 例接受 PDAc 切除术的患者,其中 236 例(26%)患者出现了 rrPDAc。每年 rrPDAc 的中位发生率为 25.3%(IQR 22-30.2%)。rrPDAc、非快速复发和无复发患者的中位生存期分别为 10.3 个月、25.2 个月和 56.1 个月(P 结论:尽管治疗手段不断进步,rrPDAc 患者的中位生存期仍然很短:尽管治疗手段不断进步,但rrPDAc的发病率仍保持不变。SSI和结节阳性与rrPDAc风险增加有独立关联,而辅助化疗则与风险降低有关。重点预防快速复发的策略可提高生存率。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Rapid metastatic recurrence after pancreatic cancer resection: a multi-center, regional analysis of trends in surgical failure over two decades
Background
Pancreatic ductal adenocarcinoma (PDAc) is a lethal malignancy, attributed in part to high rates of rapid recurrence (rrPDAc) following resection. We sought to characterize recurrence rates over time and investigate factors predictive of rrPDAc.
Methods
A regional multi-institutional cancer registry, augmented with data from the National Surgical Quality Improvement Program database, was queried for patients with PDAc from 1996 to 2020. rrPDAc was defined as recurrence within 6 months following curative-intent resection.
Results
We identified 924 patients who underwent resection for PDAc; rrPDAc occurred in 236 (26%) patients. Median incidence of rrPDAc was 25.3% (IQR 22–30.2%) per year. Median survival in rrPDAc, non-rapid recurrence, and no recurrence was 10.3, 25.2, and 56.1 months respectively (p < 0.001). Variables independently associated with greater odds of rrPDAc included surgical site infection (SSI) (OR 2.06) and nodal positivity (OR 2.05); adjuvant therapy was associated with lower odds (OR 0.38). Neoadjuvant chemotherapy did not alter risk of rrPDAc. Three-year post-recurrence survival was no different in rrPDAc versus those without.
Conclusion
Despite therapeutic advances, incidence of rrPDAc remains unchanged. SSIs and nodal positivity are independently associated with increased risk of rrPDAc, while adjuvant chemotherapy is associated with lower risk. Strategies focused on preventing rapid recurrence may improve survival.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Hpb
GASTROENTEROLOGY & HEPATOLOGY-SURGERY
CiteScore
5.60
自引率
3.40%
发文量
244
审稿时长
57 days
期刊介绍:
HPB is an international forum for clinical, scientific and educational communication.
Twelve issues a year bring the reader leading articles, expert reviews, original articles, images, editorials, and reader correspondence encompassing all aspects of benign and malignant hepatobiliary disease and its management. HPB features relevant aspects of clinical and translational research and practice.
Specific areas of interest include HPB diseases encountered globally by clinical practitioners in this specialist field of gastrointestinal surgery. The journal addresses the challenges faced in the management of cancer involving the liver, biliary system and pancreas. While surgical oncology represents a large part of HPB practice, submission of manuscripts relating to liver and pancreas transplantation, the treatment of benign conditions such as acute and chronic pancreatitis, and those relating to hepatobiliary infection and inflammation are also welcomed. There will be a focus on developing a multidisciplinary approach to diagnosis and treatment with endoscopic and laparoscopic approaches, radiological interventions and surgical techniques being strongly represented. HPB welcomes submission of manuscripts in all these areas and in scientific focused research that has clear clinical relevance to HPB surgical practice.
HPB aims to help its readers - surgeons, physicians, radiologists and basic scientists - to develop their knowledge and practice. HPB will be of interest to specialists involved in the management of hepatobiliary and pancreatic disease however will also inform those working in related fields.
Abstracted and Indexed in:
MEDLINE®
EMBASE
PubMed
Science Citation Index Expanded
Academic Search (EBSCO)
HPB is owned by the International Hepato-Pancreato-Biliary Association (IHPBA) and is also the official Journal of the American Hepato-Pancreato-Biliary Association (AHPBA), the Asian-Pacific Hepato Pancreatic Biliary Association (A-PHPBA) and the European-African Hepato-Pancreatic Biliary Association (E-AHPBA).
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


