孕产妇暴露于环境臭氧与胎儿先天性心脏缺陷:中国一项全国性多中心研究。
IF 4.7
3区 医学
Q2 ENVIRONMENTAL SCIENCES
Journal of Exposure Science and Environmental Epidemiology
Pub Date : 2024-08-31
DOI:10.1038/s41370-024-00716-4
引用次数: 0
摘要
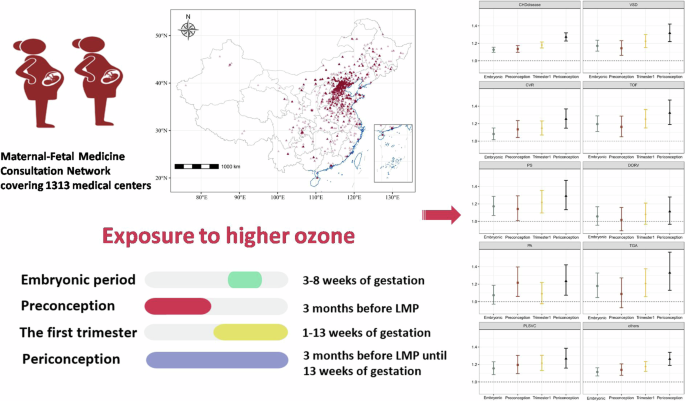
背景:在全球变暖的背景下,环境中的 O3 呈上升趋势。母体暴露于环境中的臭氧对胎儿先天性心脏缺陷(CHD)影响的现有证据仍然有限,尤其是在高污染地区:研究孕早期母体暴露于环境中的臭氧与胎儿先天性心脏病的关系:我们在中国 26 个省的 1313 家医院开展了一项全国性多中心研究,收集了 2013 年至 2021 年期间 27817 名罹患先天性心脏病的高危人群。通过从每个受试者居住区的有效网格数据集中提取每日浓度,评估了胚胎期、孕前、孕期前三个月和围孕期的环境臭氧暴露情况。根据胎儿超声心动图诊断先天性心脏病:胚胎期环境中的臭氧暴露量每增加 10 µg/m3 与合并的先天性心脏病几率增加 12.7%(几率比 [OR]:1.127,95% 置信区间 [CI]:1.098,1.155)呈近似线性相关(P 2.5 和 NO2 暴露量)。不同类型的心脏病与环境中的臭氧暴露相关的几率差别很大。我们观察到,环境中的 O3 暴露与室间隔缺损(VSD)、法洛氏四联症(TOF)、肺动脉狭窄(PS)、肺动脉闭锁(PA)、大动脉转位(TGA)和左上腔静脉持续存在(PLSVC)有明显的关联,其中 TOF 的估计值最高(OR:1.194,95% CI:1.107,1.288)。孕前、头三个月和围孕期的估计值与主要分析结果一致,表明围孕期环境中的臭氧暴露与胎儿的关系更密切:我们的研究提供的证据表明,孕早期环境中较高的臭氧浓度与胎儿先天性心脏病几率的增加有显著关联。我们的研究结果表明,孕妇、临床工作者和政策制定者需要更加关注怀孕早期暴露于较高环境臭氧的情况,以降低罹患先天性心脏病的风险,并改善整个生命周期的预后。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Maternal exposure to ambient ozone and fetal congenital heart defects: a national multicenter study in China
Ambient O3 has demonstrated an aggravated increasing trend in the context of global warming. The available evidence of maternal exposure to ambient O3 on fetal congenital heart defects (CHD) is still limited, especially in high polluted areas. To examine associations of maternal exposure to ambient O3 during early pregnancy with fetal CHDs. We conducted a national multicenter study in 1313 hospitals from 26 provinces in China and collected a total of 27,817 participants at high risk of CHD from 2013 to 2021. Exposure to ambient O3 during the embryonic period, preconception, the first trimester and periconception was assessed by extracting daily concentrations from a validated grid dataset at each subject’s residential district. CHDs were diagnosed based on fetal echocardiography. Each 10 µg/m3 increase of exposure to ambient O3 during the embryonic period was approximately linearly associated with a 12.7% (odds ratio [OR]: 1.127, 95% confidence interval [CI]: 1.098, 1.155) increase in odds of pooled CHD (p < 0.001). The associations remain robust after adjusting for ambient PM2.5 and NO2 exposure. The odds of different types of CHD in association with ambient O3 exposure varied greatly. We observed significant association of ambient O3 exposure with ventricular septal defect (VSD), tetralogy of Fallot (TOF); pulmonary stenosis (PS), pulmonary atresia (PA), transposition of great arteries (TGA) and persistent left superior vena cava (PLSVC), with TOF demonstrating the strongest estimates (OR: 1.194, 95% CI:1.107, 1.288). The estimates for preconception, the first trimester and periconception demonstrate consistent findings with the main analyses, indicating stronger associations of ambient O3 exposure during the periconception period.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
8.90
自引率
6.70%
发文量
93
审稿时长
3 months
期刊介绍:
Journal of Exposure Science and Environmental Epidemiology (JESEE) aims to be the premier and authoritative source of information on advances in exposure science for professionals in a wide range of environmental and public health disciplines.
JESEE publishes original peer-reviewed research presenting significant advances in exposure science and exposure analysis, including development and application of the latest technologies for measuring exposures, and innovative computational approaches for translating novel data streams to characterize and predict exposures. The types of papers published in the research section of JESEE are original research articles, translation studies, and correspondence. Reported results should further understanding of the relationship between environmental exposure and human health, describe evaluated novel exposure science tools, or demonstrate potential of exposure science to enable decisions and actions that promote and protect human health.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


