透析液钠与肾内高血压患者的短期血压变化:随机交叉研究。
IF 2.7
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
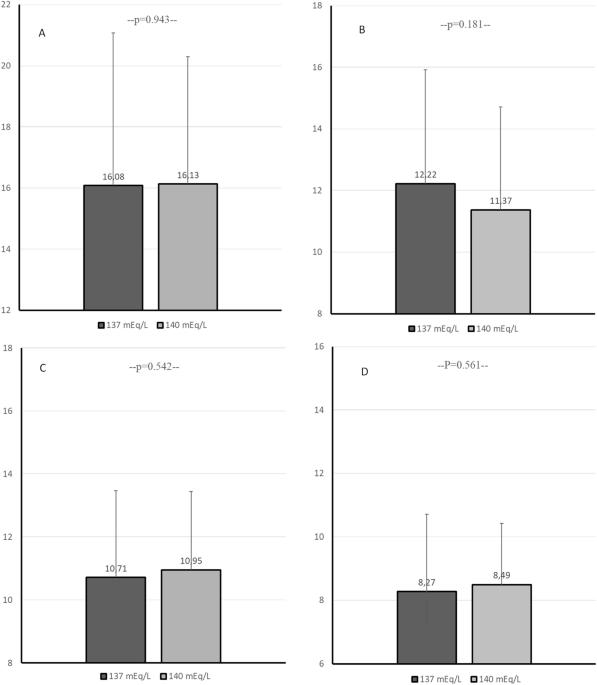
血压(BP)变异性(BPV)增加与血液透析中的心血管高风险有关。与无此症状的血液透析患者相比,析出内高血压(IDH)患者的心血管风险也会增加。非药物降压干预对该人群 BPV 的影响尚不清楚。本分析评估了低浓度(137mEq/L)与标准浓度(140mEq/L)透析液钠对 IDH 患者短期 BPV 的影响。29 名 IDH 患者以随机交叉方式接受了 4 次低浓度(137mEq/L)血液透析,然后接受了 4 次标准(140mEq/L)透析液钠浓度血液透析,反之亦然。从第 4 次透析开始,每种透析液钠均进行 48 小时动态血压测量。计算了 48 小时、24 小时、白天和夜间的血压变异指数。与标准透析液钠浓度相比,低浓度透析液钠的 48 小时平均血压降低了 5.3/2.6 mmHg(分别为 p = 0.005/p = 0.007)。低浓度透析液钠与标准透析液钠相比,所有 48 小时收缩压 BPV 指数均无显著差异(SBP-SD:16.99 ± 5.39 vs. 16.98 ± 4.33 mmHg,p = 0.982;SBP-wSD:15.93 ± 5.02 vs. 16.12 ± 4.16 mmHg,p = 0.769;SBP-ARV:11.99 ± 3.67 vs. 11.45 ± 3.35 mmHg,p = 0.392;SBP-CV:12.36 ± 3.65 vs. 11.92 ± 3.18%,p = 0.302,分别为低透析液钠与标准透析液钠)。低透析液钠的舒张压 BPV 指数在数值上较低,但在统计学上并不低。总体而言,在一些比较中观察到了明显的差异,低透析液钠的趋势是白天 2 的 BPV 较低,夜间 2 的 BVP 较高。总之,低透析液钠浓度不会影响 IDH 患者的 BPV 水平。未来的研究应探索其他干预措施,以降低这一高风险人群的血压和血压变压。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Dialysate sodium and short-term blood pressure variability in patients with intradialytic hypertension: a randomized crossover study
Increased blood pressure (BP) variability (BPV) is associated with high cardiovascular risk in hemodialysis. Patients with intradialytic hypertension (IDH) also exhibit an increased cardiovascular risk compared to hemodialysis patients without this condition. The impact of non-pharmacological BP-lowering interventions on BPV in this population remains unknown. This analysis evaluated the effect of low (137mEq/L) compared to standard (140mEq/L) dialysate sodium concentration on short-term BPV in patients with IDH. In a randomized cross-over manner, 29 IDH patients underwent 4 hemodialysis sessions with low (137mEq/L) followed by 4 sessions with standard (140mEq/L) dialysate sodium or vice versa. 48 h ambulatory BP measurement was performed from the start of the 4th session on each dialysate sodium. BPV indices during the 48 h, 24 h, day-time and night-time periods were calculated. Mean 48 h BP was 5.3/2.6 mmHg lower with low compared to standard dialysate sodium concentration, (p = 0.005/p = 0.007 respectively). All 48 h systolic BPV indices examined showed non-significant differences between low and standard dialysate sodium (SBP-SD: 16.99 ± 5.39 vs. 16.98 ± 4.33 mmHg, p = 0.982; SBP-wSD: 15.93 ± 5.02 vs. 16.12 ± 4.16 mmHg, p = 0.769; SBP-ARV: 11.99 ± 3.67 vs. 11.45 ± 3.35 mmHg, p = 0.392; SBP-CV: 12.36 ± 3.65 vs. 11.92 ± 3.18%, p = 0.302, with low vs. standard dialysate sodium, respectively). Diastolic BPV indices were numerically, but not statistically, lower with low dialysate sodium. Overall, significant differences were observed in some comparisons with a trend for lower BPV during day-time 2 and higher BVP during night-time 2 with low dialysate sodium. In conclusion, low dialysate sodium concentration does not affect BPV levels in patients with IDH. Future research should explore alternative interventions to reduce BP and BPV in this high-risk population.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


