小特发性毛细血管瘤玻璃体切除术(SMALL)研究:传统内缘膜剥离与倒置皮瓣。
IF 3.2
3区 医学
Q1 OPHTHALMOLOGY
引用次数: 0
摘要
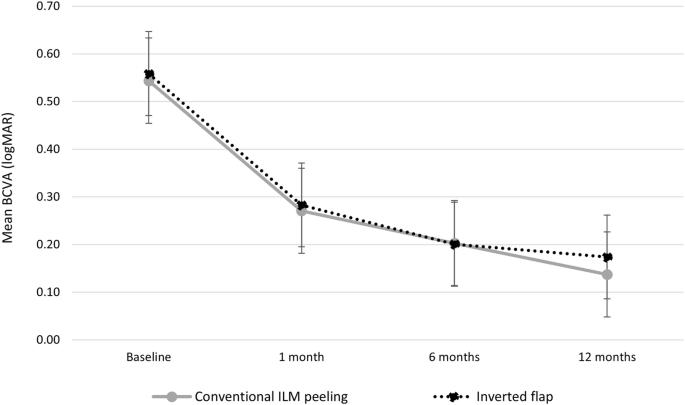
背景:比较传统的内缘膜(ILM)剥离与倒瓣技术在特发性小黄斑孔中的应用:比较小特发性黄斑孔的传统内缘膜(ILM)剥离与倒置瓣技术:回顾性多中心队列研究,包括对≤250 μm 的特发性黄斑孔进行原发性玻璃体切除术的连续病例。主要结果是最佳矫正视力(BCVA)变化和黄斑孔闭合率。光学相干断层扫描(OCT)上的闭合模式以及外缘膜(ELM)和椭圆体区(EZ)的恢复率被视为次要结果:传统ILM剥离组和倒置皮瓣组分别共有389和250只眼睛。两组的闭孔率相当(ILM剥离组为98.5%,倒置皮瓣组为97.6%)。基线时,两组的平均 BCVA 值相当(p = 0.331)。12 个月时,传统 ILM 剥离组的平均 BCVA 为 0.14 ± 0.19 logMAR,倒置皮瓣组为 0.17 ± 0.18 logMAR(p = 0.08)。12个月时,传统ILM剥离组73%的眼睛呈U形闭合形态,而倒置皮瓣组为55%。12个月时,传统ILM剥离组和倒置皮瓣组的ELM恢复率分别为96%和86%(P 结论:传统ILM剥离组和倒置皮瓣组的ELM恢复率分别为96%和86%:在特发性小黄斑孔手术中,倒置皮瓣技术在视觉效果和闭合率方面没有优势。此外,与传统剥离法相比,这种技术似乎会影响术后视网膜外层的恢复。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Vitrectomy in Small idiopathic MAcuLar hoLe (SMALL) study: conventional internal limiting membrane peeling versus inverted flap
To compare conventional internal limiting membrane (ILM) peeling versus inverted flap technique in small idiopathic macular hole. Retrospective, multicentre cohort study including consecutive eyes with a ≤250 μm idiopathic macular hole treated with primary vitrectomy. The primary outcome was best-corrected visual acuity (BCVA) change and macular hole closure rate. Closure patterns on optical coherence tomography (OCT) and rates of external limiting membrane (ELM) and ellipsoid zone (EZ) recovery were considered as secondary outcomes. A total of 389 and 250 eyes were included in the conventional ILM peeling group and in the inverted flap group, respectively. Hole closure rate was comparable between the two groups (98.5% in the ILM peeling group and 97.6% in the inverted flap group). Mean BCVA was comparable between the two groups at baseline (p = 0.331). At 12 months, mean BCVA was 0.14 ± 0.19 logMAR in the conventional ILM peeling group and 0.17 ± 0.18 logMAR in the inverted flap group (p = 0.08). At 12 months, 73% of eyes had a U-shape closure morphology in the conventional ILM peeling group versus 55% in the inverted flap group. At 12 months, ELM recovery rate was 96% and 86% in the conventional ILM peeling group and in the inverted flap group, respectively (p < 0.001); EZ recovery rate was 78% and 69%, respectively (p = 0.04). The inverted flap technique provides no advantages in terms of visual outcome and closure rate in small idiopathic macular hole surgery. Additionally, this technique seems to impair postoperative restoration of external retinal layers compared with conventional peeling.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Eye
医学-眼科学
CiteScore
6.40
自引率
5.10%
发文量
481
审稿时长
3-6 weeks
期刊介绍:
Eye seeks to provide the international practising ophthalmologist with high quality articles, of academic rigour, on the latest global clinical and laboratory based research. Its core aim is to advance the science and practice of ophthalmology with the latest clinical- and scientific-based research. Whilst principally aimed at the practising clinician, the journal contains material of interest to a wider readership including optometrists, orthoptists, other health care professionals and research workers in all aspects of the field of visual science worldwide. Eye is the official journal of The Royal College of Ophthalmologists.
Eye encourages the submission of original articles covering all aspects of ophthalmology including: external eye disease; oculo-plastic surgery; orbital and lacrimal disease; ocular surface and corneal disorders; paediatric ophthalmology and strabismus; glaucoma; medical and surgical retina; neuro-ophthalmology; cataract and refractive surgery; ocular oncology; ophthalmic pathology; ophthalmic genetics.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


