幽门螺杆菌对袖状胃切除术的影响以及肥胖和糖尿病患者胃微生物组的差异。
IF 4.2
2区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
摘要
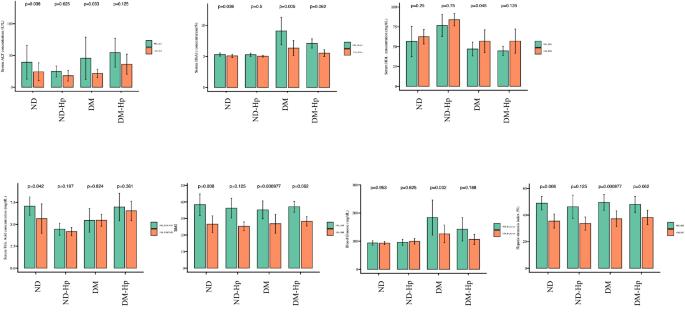
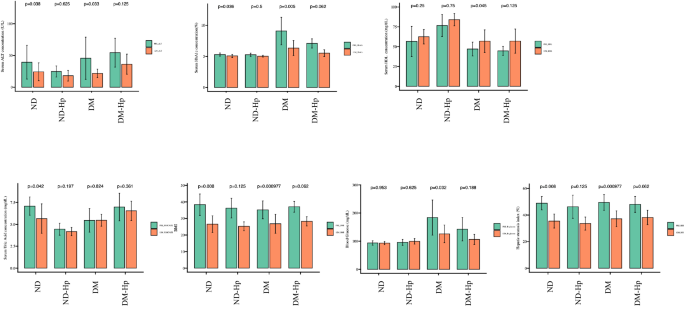
背景:肥胖症和糖尿病(DM)已成为全球关注的公共卫生问题。这两种疾病都会造成严重后果,并带来巨大的医疗成本和生产力损失。此外,幽门螺杆菌感染可能是导致这些疾病的风险因素。然而,根除幽门螺杆菌感染是否会直接导致体重减轻或改善胰岛素敏感性还不得而知:在这项研究中,我们根据 40 名肥胖、DM 和幽门螺杆菌感染患者的胃微生物群状况,确认了袖状胃切除术的效果。通过 16S V3-V4 测序,肥胖症患者被分为四组:无幽门螺杆菌感染的非 DM 组(ND)、有幽门螺杆菌感染的非 DM 组(ND-HP)、DM 组和有幽门螺杆菌感染的 DM 组(DM-HP):结果:在 DM 组中,ALT、血红蛋白、HbA1c、血糖和 HSI 显著降低,而高密度脂蛋白显著升高。幽门螺杆菌阳性组则无明显差异。胃微生物群的多样性按照 ND > DM > ND-HP > DM-HP 组的顺序下降。我们还对术前微生物和临床数据进行了相关性分析。在 ND-HP 组中,前 20 个胃微生物群大多与糖代谢呈负相关。然而,幽门螺杆菌感染与术前胰岛素水平呈正相关:因此,这些研究结果表明,肥胖症和糖尿病患者显然能从手术中获益,但幽门螺杆菌感染也可能影响临床改善。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Effect of Helicobacter pylori on sleeve gastrectomy and gastric microbiome differences in patients with obesity and diabetes
Obesity and diabetes mellitus (DM) have become public health concerns worldwide. Both conditions have severe consequences and are associated with significant medical costs and productivity loss. Additionally, Helicobacter pylori infection may be a risk factor for the development of these conditions. However, whether eradicating H. pylori infection directly causes weight loss or improves insulin sensitivity is unknown. In this study, we confirmed the effect of sleeve gastrectomy according to the state of the gastric microbiota in 40 patients with obesity, DM, and H. pylori infection. Patients with obesity were divided into four groups: non-DM without H. pylori infection (ND), non-DM with H. pylori infection (ND-HP), DM, and DM with H. pylori infection (DM-HP) using 16S V3–V4 sequencing. In the DM group, ALT, hemoglobin, HbA1c, blood glucose, and HSI significantly decreased, whereas high-density lipoprotein significantly increased. However, in the H. pylori-positive group, no significant difference was observed. The diversity of gastric microbiota decreased in the order of the ND > DM > ND-HP > DM-HP groups. We also conducted a correlation analysis between the preoperative microbes and clinical data. In the ND-HP group, most of the top 20 gastric microbiota were negatively correlated with glucose metabolism. However, H. pylori infection was positively correlated with pre-insulin levels. Therefore, these findings indicate that patients with obesity and diabetes clearly benefit from surgery, but H. pylori infection may also affect clinical improvement.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

International Journal of Obesity
医学-内分泌学与代谢
CiteScore
10.00
自引率
2.00%
发文量
221
审稿时长
3 months
期刊介绍:
The International Journal of Obesity is a multi-disciplinary forum for research describing basic, clinical and applied studies in biochemistry, physiology, genetics and nutrition, molecular, metabolic, psychological and epidemiological aspects of obesity and related disorders.
We publish a range of content types including original research articles, technical reports, reviews, correspondence and brief communications that elaborate on significant advances in the field and cover topical issues.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


