孕前或孕期诊断出的慢性高血压及其对妊娠结果的影响。
IF 2.7
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
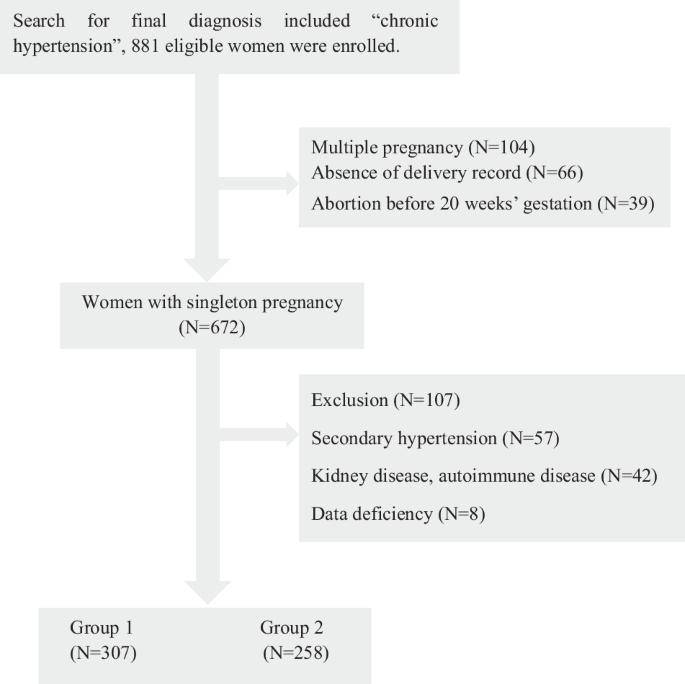
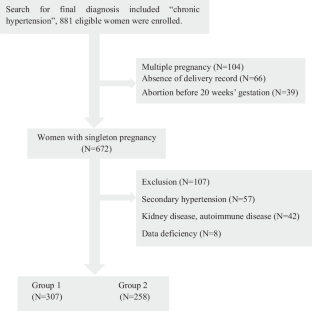
妊娠期慢性高血压(CH)在最初 20 周前或 20 周内发现,根据诊断时间的不同,其风险也不同。这项真实世界研究于2018年1月至2023年6月进行,纳入了患有CH的单胎妊娠,对孕前CH(第1组)和新诊断的CH(第2组)进行比较。共有 565 名妇女参与了最终分析,其中 307 人在第一组中患有孕前妊娠合并症,258 人在第二组中患有新发妊娠合并症。第一组中更多的人患有妊娠前糖尿病和妊娠高血压病史,而第二组中妊娠体重增加过多的发生率更高。值得注意的是,56.2%的第 2 组患者在 20 周前没有接受降压治疗,而第 1 组的这一比例为 36.2%,这导致了基线血压的显著差异。研究显示,与第一组相比,第二组先兆子痫(44.2% 对 34.9%)和胎盘早剥(5.4% 对 2.0%)的发病率更高。 这些研究结果表明,与孕前确诊的孕妇相比,在孕前 20 周新确诊 CH 的孕妇面临的不良后果更多。加强监测和尽早干预可能有助于控制新发CH的孕妇。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Chronic hypertension diagnosed before or during pregnancy and its effects on pregnancy outcomes
Chronic hypertension (CH) during pregnancy, identified before or within the first 20 weeks, presents varying risks depending on the timing of diagnosis. This real-world study was conducted from January 2018 to June 2023 and included singleton pregnancies with CH to compare pre-pregnancy CH (Group 1) and newly diagnosed CH (Group 2). There were 565 women in the final analysis, with 307 in Group 1 with pre-pregnancy CH and 258 in Group 2 with new-onset CH. Those in Group 1 more frequently had pre-gestational diabetes and a history of hypertensive disorders in pregnancy, whereas Group 2 had a higher incidence of excessive gestational weight gain. Notably, 56.2% of Group 2 patients did not receive antihypertensive treatment before 20 weeks, while the proportion was 36.2% in Group 1, resulting in a significant difference in baseline blood pressure. The study revealed higher incidences of preterm preeclampsia (44.2% vs. 34.9%) and placental abruption (5.4% vs. 2.0%) in Group 2 compared to Group 1. After adjustment, logistic regression indicated that Group 2 had a 1.8-fold higher risk of preterm preeclampsia than Group 1. These findings suggest that pregnant women newly diagnosed with CH in the first 20 weeks face increased adverse outcomes compared to those diagnosed before pregnancy. Intense monitoring and earlier intervention may help manage women with new-onset CH.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


