体重指数的个体内变异性越大,与 COVID-19 相关的住院和 COVID 后病症的风险就越高。
IF 3.8
2区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
摘要
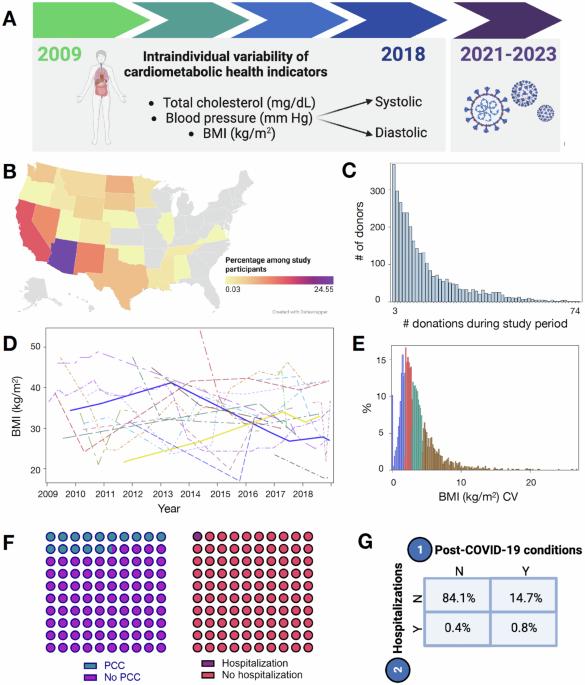
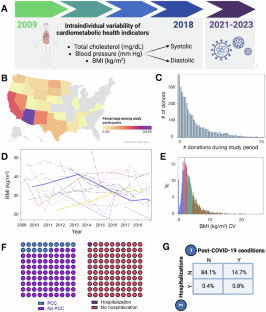
背景:心脏代谢疾病是导致 COVID-19 严重程度的危险因素。心脏代谢健康在多大程度上可作为减轻 SARS-CoV-2 短期和长期后果的可调节因素仍不清楚。我们的目的是在相对健康的人群中评估心脏代谢健康指标的个体内变异性与 COVID-19 相关住院和 COVID 后病症(PCC)之间的关联:这项回顾性、多地点队列研究是一项事后分析,研究对象是在美国 24 个州(2009-2018 年)的常规献血访问中收集了心脏代谢健康数据,并回答了 COVID-19 问卷(2021-2023 年)的个人。血压(收缩压、舒张压)、总循环胆固醇和体重指数(BMI)的个体内变异性被定义为所有可用献血时间点(从 3 到 74)的变异系数(CV);参与者被分为 CV 四分位数。相关性通过多变量二项回归进行评估:总共有 3344 名参与者提供了 42,090 次捐赠(中位数为 9 [IQR 5, 17])。首次捐赠时的中位年龄为 48 岁(38 岁,56 岁)。1.2%(N = 40)因 COVID-19 而住院,15.5%(N = 519)患有 PCC。BMI 变异性越大,COVID-19 住院风险越高(第四四分位 aRR 4.15 [95% CI 1.31, 13.11],p = 0.02;第三四分位 aRR 3.41 [95% CI 1.09, 10.69],p = 0.04)。体重指数变异性较高的参与者患 PCC 的风险更大(第四四分位数 aRR 1.29 [95% CI 1.02, 1.64];p = 0.04)。血压(收缩压、舒张压)和总循环胆固醇的个体内变异性与 COVID-19 住院或 PCC 风险无关(所有 p > 0.05)。从因果中介分析来看,BMI变异性最高的四分位数与PCC之间的关系与住院无关(P > 0.05):结论:BMI的个体内变异性越高,COVID-19住院和PCC风险越大。我们的研究结果表明,有必要进一步阐明解释这些关联的机制以及持续保持体重的重要性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Higher intraindividual variability of body mass index is associated with elevated risk of COVID-19 related hospitalization and post-COVID conditions
Cardiometabolic diseases are risk factors for COVID-19 severity. The extent that cardiometabolic health represents a modifiable factor to mitigate the short- and long-term consequences from SARS-CoV-2 remains unclear. Our objective was to evaluate the associations between intraindividual variability of cardiometabolic health indicators and COVID-19 related hospitalizations and post-COVID conditions (PCC) among a relatively healthy population. This retrospective, multi-site cohort study was a post-hoc analysis among individuals with cardiometabolic health data collected during routine blood donation visits in 24 US states (2009-2018) and who responded to COVID-19 questionnaires (2021–2023). Intraindividual variability of blood pressure (systolic, diastolic), total circulating cholesterol, and body mass index (BMI) were defined as the coefficient of variation (CV) across all available donation timepoints (ranging from 3 to 74); participants were categorized into CV quartiles. Associations were evaluated by multivariable binomial regressions. Overall, 3344 participants provided 42,090 donations (median 9 [IQR 5, 17]). The median age was 48 years (38, 56) at the first study donation. 1.2% (N = 40) were hospitalized due to COVID-19 and 15.5% (N = 519) had PCC. Higher BMI variability was associated with greater risk of COVID-19 hospitalization (4th quartile aRR 4.15 [95% CI 1.31, 13.11], p = 0.02; 3rd quartile aRR 3.41 [95% CI 1.09, 10.69], p = 0.04). Participants with higher variability of BMI had greater risk of PCC (4th quartile aRR 1.29 [95% CI 1.02, 1.64]; p = 0.04). Intraindividual variability of blood pressure (systolic, diastolic) and total circulating cholesterol were not associated with COVID-19 hospitalization or PCC risk (all p > 0.05). From causal mediation analysis, the association between the highest quartiles of BMI variability and PCC was not mediated by hospitalization (p > 0.05). Higher intraindividual variability of BMI was associated with COVID-19 hospitalization and PCC risk. Our findings underscore the need for further elucidating mechanisms that explain these associations and importance for consistent maintenance of body weight.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

International Journal of Obesity
医学-内分泌学与代谢
CiteScore
10.00
自引率
2.00%
发文量
221
审稿时长
3 months
期刊介绍:
The International Journal of Obesity is a multi-disciplinary forum for research describing basic, clinical and applied studies in biochemistry, physiology, genetics and nutrition, molecular, metabolic, psychological and epidemiological aspects of obesity and related disorders.
We publish a range of content types including original research articles, technical reports, reviews, correspondence and brief communications that elaborate on significant advances in the field and cover topical issues.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


