导管肾上腺消融术治疗双侧原发性醛固酮增多症的合理性和意义。
IF 4.3
2区 医学
Q1 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
矿物皮质激素受体拮抗剂(MRA)治疗双侧原发性醛固酮增多症(PA)是指南推荐的主要方案,但由于副作用多,患者依从性差。我们旨在研究导管肾上腺消融术是否可作为双侧 PA 的替代治疗方法。644 名 PA 患者来自 6054 名高血压患者,均接受了肾上腺 CT 扫描和肾上腺静脉采样(AVS),以进行 PA 亚型分类。根据原发性醛固酮增多症手术疗效(PASO)标准,对治疗后6个月的临床和生化疗效进行了评估。根据AVS结果,93名PA患者接受了肾上腺消融术治疗,其中包括25名双侧PA患者和68名单侧PA患者。与基线水平相比,办公室SBP和DBP明显下降,血清钾水平升高,ARR明显下降(p本文章由计算机程序翻译,如有差异,请以英文原文为准。
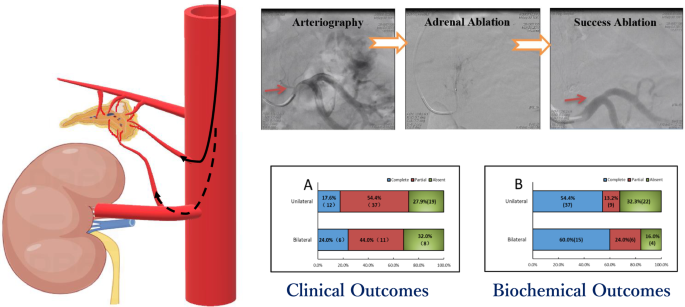

Rationality and implication of catheter-based adrenal ablation for bilateral primary aldosteronism
Mineralocorticoid receptor antagonists (MRAs) for bilateral primary aldosteronism (PA) are the mainstay option recommended by guidelines, but poor compliance occurs due to numerous side effects. We aimed to examine whether catheter-based adrenal ablation could be an alternative treatment for bilateral PA.644 PA patients were included from a total of 6054 hypertensive patients. Adrenal CT scan and adrenal venous sampling (AVS) were both performed for PA subtype classification. Clinical and biochemical outcomes were assessed at 6 months after treatment according to the Primary Aldosteronism Surgical Outcome (PASO) criteria.93 patients with PA were recruited to be treated by adrenal ablation, including 25 bilateral PA and 68 unilateral PA according to AVS results. Office SBP and DBP significantly decreased from baseline levels, serum potassium levels increased and ARR significantly decreased (p < 0.01) in both the bilateral and unilateral groups. In the bilateral group, complete, partial and absent clinical success was achieved in 6 (24.0%), 11 (44.0%) and 8(32.0%) patients, respectively. In the unilateral group, complete, partial and absent clinical success was achieved in 12 (17.6%), 37 (54.4%), and 19 (27.9%) patients, respectively. The numbers of patients achieving complete, partial, and absent biochemical success were 15 (60.0%), 6 (24.0%), and 4 (16.0%), respectively, in the bilateral group versus 37 (54.4%), 9 (13.2%), and 22 (32.3%), respectively, in the unilateral group. In conclusion, we provide evidence for the beneficial outcomes of unilateral adrenal ablation for patients with bilateral PA. Our findings provide insight into an alternative option for patients with bilateral excess aldosterone.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Hypertension Research
医学-外周血管病
CiteScore
7.40
自引率
16.70%
发文量
249
审稿时长
3-8 weeks
期刊介绍:
Hypertension Research is the official publication of the Japanese Society of Hypertension. The journal publishes papers reporting original clinical and experimental research that contribute to the advancement of knowledge in the field of hypertension and related cardiovascular diseases. The journal publishes Review Articles, Articles, Correspondence and Comments.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


