肥胖和脂肪组织功能障碍在骨关节炎疼痛中的作用。
IF 29.4
1区 医学
Q1 RHEUMATOLOGY
引用次数: 0
摘要
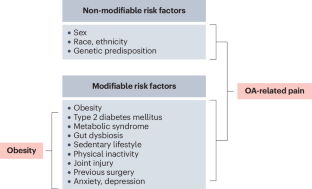
肥胖在骨关节炎(OA)相关疼痛中起着关键和多方面的作用,其影响超出了体重指数(BMI)的机理。肥胖通过与 OA 相关疼痛有关的各种可改变的风险因素直接或间接地产生影响。脂肪组织功能障碍通过局部和全身炎症、免疫功能障碍以及促炎症细胞因子和脂肪因子的产生,与 OA 相关疼痛密切相关。脂肪组织功能障碍与代谢综合征有着错综复杂的联系,代谢综合征对 OA 相关疼痛具有独立的特定影响,有别于与体重指数的关联。肥胖、脂肪组织功能障碍和代谢综合征之间的相互作用通过不同的疼痛机制(包括痛觉疼痛、外周敏感化和中枢敏感化)影响 OA 相关疼痛。这些复杂的相互作用导致 OA 和肥胖症患者的疼痛体验加剧。此外,肥胖症患者的疼痛管理策略效率较低。重要的是,针对肥胖和代谢综合征的治疗干预有望控制 OA 相关疼痛。深入了解肥胖、代谢综合征和 OA 相关疼痛之间错综复杂的关系至关重要,这对改善疼痛管理和开发 OA 创新治疗方案具有重要意义。本文章由计算机程序翻译,如有差异,请以英文原文为准。
The role of obesity and adipose tissue dysfunction in osteoarthritis pain
Obesity has a pivotal and multifaceted role in pain associated with osteoarthritis (OA), extending beyond the mechanistic influence of BMI. It exerts its effects both directly and indirectly through various modifiable risk factors associated with OA-related pain. Adipose tissue dysfunction is highly involved in OA-related pain through local and systemic inflammation, immune dysfunction, and the production of pro-inflammatory cytokines and adipokines. Adipose tissue dysfunction is intricately connected with metabolic syndrome, which independently exerts specific effects on OA-related pain, distinct from its association with BMI. The interplay among obesity, adipose tissue dysfunction and metabolic syndrome influences OA-related pain through diverse pain mechanisms, including nociceptive pain, peripheral sensitization and central sensitization. These complex interactions contribute to the heightened pain experience observed in individuals with OA and obesity. In addition, pain management strategies are less efficient in individuals with obesity. Importantly, therapeutic interventions targeting obesity and metabolic syndrome hold promise in managing OA-related pain. A deeper understanding of the intricate relationship between obesity, metabolic syndrome and OA-related pain is crucial and could have important implications for improving pain management and developing innovative therapeutic options in OA. In this Review, the authors explore the complex interactions between osteoarthritis-related pain and obesity, adipose tissue dysfunction and metabolic syndrome, and discuss how knowledge of these relationships could help improve pain management and identify new therapeutic options.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Nature Reviews Rheumatology
医学-风湿病学
CiteScore
29.90
自引率
0.90%
发文量
137
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Rheumatology is part of the Nature Reviews portfolio of journals. The journal scope covers the entire spectrum of rheumatology research. We ensure that our articles are accessible to the widest possible audience.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


