治愈患者中的顽固性静脉曲张:了解肝静脉压力梯度的作用
IF 9.5
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
背景& 目的去除致病因子(ER)可促进肝硬化门脉高压的恢复和改善。尽管ER后肝静脉压阶差(HVPG)降至10 mmHg以下,但仍有患者发现食管静脉曲张(EV)和门脉分流(PSS),这对ER时HVPG反映真实门脉压力的准确性提出了质疑。方法这是一项双中心 "概念验证 "研究,对至少 5 年ER 后仍有静脉曲张且 HVPG≥10 mmHg 的 HCV 或酒精相关肝硬化患者的 HVPG 和超声引导下经皮 DPP 进行评估。结果纳入了 7 名患有 HCV 的患者和 3 名患有酒精相关肝硬化的患者,这些患者均患有顽固性静脉曲张,且在接受 ER 至少 5 年后 HVPG <10 mmHg。在评估时,所有患者的门静脉均通畅,并得到代偿。血小板计数中位数为 129.5(IQR 95-145)×109/ml,肝硬度测量中位数为 16.15(IQR 14.4-22.3)kPa。五名患者的EV大小保持不变(两大三小),五名患者的EV在急诊室手术后缩小为小EV。楔形肝静脉压(中位数 19 [IQR 16.5-20] mmHg)和门静脉压(中位数 18 [IQR 15-19.5] mmHg)具有极好的相关性(R = 0.93,p <0.0001)。门静脉压力梯度(PPG)证实,所有患者均无 HVPG 发现的临床意义上的门静脉高压。ER 后,尽管 HVPG 为 10 mmHg,但 EV 仍可能持续存在。对于 EV 和 HVPG <10 mmHg 患者,预防性治疗的益处尚不清楚。影响和意义:尽管去除致病因素后病情发展良好,但一些患者的静脉曲张仍持续存在,目前缺乏评估和管理这类人群门静脉高压症的简明指南。我们的研究强调了在没有临床显著门静脉高压的情况下静脉曲张的持续存在,并显著证明了肝静脉压力梯度(HVPG)在反映这一特殊患者群体的门静脉压力方面的准确性。这些发现强调了 HVPG 在病因去除后评估门静脉高压中的关键作用,并为进一步研究临床结果和去除病因后静脉曲张持续存在者使用非选择性β-受体阻滞剂的必要性奠定了基础。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Persistent varices in cured patients: Understanding the role of hepatic venous pressure gradient
Background & Aims
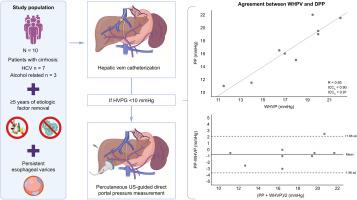
Etiologic factor removal (ER) drives recompensation and improves portal hypertension in cirrhosis. Esophageal varices (EV) and portosystemic shunts (PSS) have been found in patients despite hepatic venous pressure gradient (HVPG) dropping below 10 mmHg after ER, questioning HVPG accuracy in reflecting true portal pressure in the setting of ER. We aim to evaluate the correlation of HVPG with direct portal pressure (DPP) in patients with persistence of EV after ER despite HVPG <10 mmHg.
Methods
This is a bicentric ‘proof of concept’ study evaluating HVPG and ultrasound-guided percutaneous DPP in patients with HCV or alcohol-related cirrhosis with persistent varices and HVPG <10 mmHg after at least 5 years of ER.
Results
Seven patients with HCV and three with alcohol-related cirrhosis with persistent varices and HVPG <10 mmHg after at least 5 years of ER were included. At evaluation, all patients had a patent portal vein and were compensated. The median platelet count was 129.5 (IQR 95–145) × 109/ml, and the median liver stiffness measurement was 16.15 (IQR 14.4–22.3) kPa. In five patients, EV remained the same size (two large and three small), and five downsized to small after ER. Wedge hepatic vein pressure (median 19 [IQR 16.5–20] mmHg) and portal pressure (median 18 [IQR 15–19.5] mmHg) had an excellent correlation (R = 0.93, p <0.0001). Portal pressure gradient (PPG) confirmed the absence of clinically significant portal hypertension as identified by HVPG across all the patients.
Conclusions
HVPG accurately reflects PPG in the context of HCV and alcohol-related cirrhosis regression. After ER, EV may persist despite HVPG <10 mmHg. The benefit of prophylaxis in patients with EV and HVPG <10 mmHg is unknown. Future studies with clinical endpoints are needed to validate our findings.
Impact and implications:
Despite a favorable evolution after the removal of the etiologic factor, varices persist in some patients, and there is a lack of concise guidelines for the evaluation and management of portal hypertension in this population. Our research underscores the persistence of varices in the absence of clinically significant portal hypertension and significantly demonstrates the accuracy of hepatic venous pressure gradient (HVPG) in reflecting portal vein pressure in this specific patient group. These findings emphasize the crucial role of HVPG in the assessment of portal hypertension after etiologic factor removal and lay the groundwork for further investigation into clinical outcomes and the necessity of non-selective beta-blockers in individuals with persistent varices after the removal of etiologic factor.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

JHEP Reports
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
12.40
自引率
2.40%
发文量
161
审稿时长
36 days
期刊介绍:
JHEP Reports is an open access journal that is affiliated with the European Association for the Study of the Liver (EASL). It serves as a companion journal to the highly respected Journal of Hepatology.
The primary objective of JHEP Reports is to publish original papers and reviews that contribute to the advancement of knowledge in the field of liver diseases. The journal covers a wide range of topics, including basic, translational, and clinical research. It also focuses on global issues in hepatology, with particular emphasis on areas such as clinical trials, novel diagnostics, precision medicine and therapeutics, cancer research, cellular and molecular studies, artificial intelligence, microbiome research, epidemiology, and cutting-edge technologies.
In summary, JHEP Reports is dedicated to promoting scientific discoveries and innovations in liver diseases through the publication of high-quality research papers and reviews covering various aspects of hepatology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


