评估初级经皮冠状动脉介入治疗后稳定 ST 段抬高型心肌梗死患者早期返院的安全性
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
背景ST段抬高型心肌梗死(STEMI)患者在接受初级经皮冠状动脉介入治疗(PPCI)后返院在地区医疗保健项目中很常见。我们研究了稳定型 STEMI 患者 PPCI 后早期返院的短期和长期安全性。方法纳入了 2016 年至 2018 年期间在弗雷泽卫生局接受 PPCI 的连续稳定型 STEMI 患者。比较了早期和非遣返队列的结果。共同主要结局是30天和1年后的死亡、心肌梗死、充血性心力衰竭和中风的复合结果。研究人员进行了逻辑回归分析,以确定早期遣返与预后之间的关系,并评估转院至心脏病专家与内科医生护理中心的影响。 结果 共纳入了 788 名患者,其中 62% 的患者被提前遣返。两组患者的主要综合结果和个体结果率相似。早期遣返并不是30天(赔率[OR] 0.93,95% 置信区间[CI] 0.50-1.72;P = 0.82)或1年(OR 1.05,95% CI 0.67-1.65;P = 0.8)主要结局或30天(OR 1.35,95% CI 0.41-4.47,P = 0.63)或1年(OR 1.03,95% CI 0.44-2.40;P = 0.95)死亡率的独立预测因素。结论PPCI术后稳定型STEMI患者的早期转运从短期和长期结果来看似乎是安全的,转运至内科中心与转运至心脏病中心并不影响结果。PPCI术后,早期转运可将稳定的STEMI患者重新分配到地区性医院的低急诊环境中。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Assessing the Safety of Early Repatriation for Stable ST-Segment Elevation Myocardial Infarction Patients After Primary Percutaneous Coronary Intervention
Background
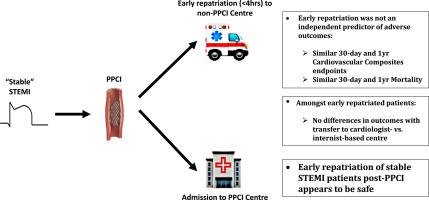
Repatriation of ST-segment elevation myocardial infarction (STEMI) patients after primary percutaneous coronary intervention (PPCI) is common in regional health care programs. We examined the short- and long-term safety of early repatriation after PPCI in stable STEMI patients.
Methods
Consecutive stable STEMI patients undergoing PPCI between 2016 to 2018 in the Fraser Health Authority were included. Outcomes were compared between early and nonrepatriated cohorts. Co-primary outcomes were a composite of death, myocardial infarction, congestive heart failure, and stroke at 30 days and 1 year. Logistic regression analyses were performed to determine association between early repatriation and outcomes, and to assess impact of transfer to cardiologist- vs internist-based care centres.
Results
A total of 788 patients were included, with 62% being repatriated early. Primary composite and individual outcomes rates were similar between both cohorts. Early repatriation was not an independent predictor of 30-day (odds ratio [OR] 0.93, 95% confidence interval [CI] 0.50-1.72; P = 0.82) or 1-year (OR 1.05, 95% CI 0.67-1.65; P = 0.8) primary outcome, or of 30-day (OR 1.35, 95% CI 0.41-4.47, P = 0.63) or 1-year (OR 1.03, 95% CI 0.44-2.40; P = 0.95) mortality. Among early repatriated patients, transfer to cardiologist- vs internist-based care centres was not an independent factor for 30-day (OR 1.07, 95% CI 0.45-2.54; P = 0.87) or 1-year (OR 1.17, 95% 0.55-2.50, P = 0.69) primary outcome.
Conclusions
Early repatriation of stable STEMI patients after PPCI appears to be safe based on short- and long-term outcomes, and transfer to internist- vs cardiology-based centres did not affect outcomes. After PPCI, early repatriation allows for redistribution of stable STEMI patients to lower-acuity settings across regional hospitals.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

CJC Open
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
3.30
自引率
0.00%
发文量
143
审稿时长
60 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


