原发性醛固酮增多症中单侧醛固酮增多症的发病率:新型化学发光免疫测定法对日本血浆醛固酮测量的影响。
IF 4.3
2区 医学
Q1 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
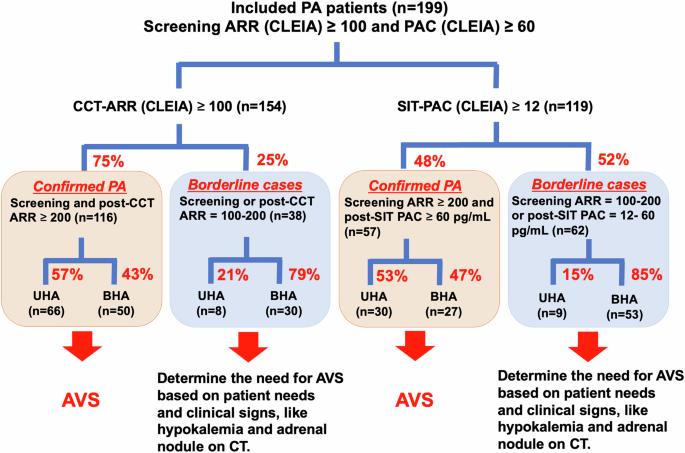
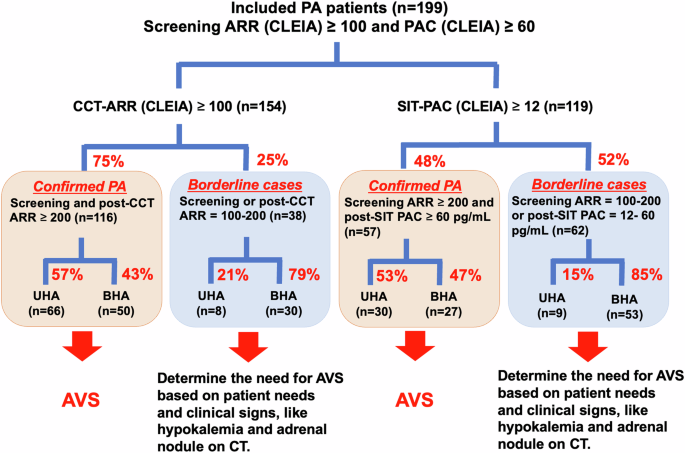
本研究旨在评估原发性醛固酮增多症(PA)患者中单侧醛固酮过多症(UHA)的发病率及其临床特征,原发性醛固酮增多症是通过化学发光酶免疫测定法(CLEIA)测定血浆醛固酮浓度(PAC)确诊的。我们回顾性分析了日本原发性醛固酮增多症研究 II(JPAS II)数据集中 199 例 PA 患者的数据,其中包括接受肾上腺静脉采样(AVS)、卡托普利挑战试验(CCT)和/或生理盐水输注试验(SIT)并通过 CLEIA 测定 PAC 的患者。根据日本内分泌学会关于 PA 诊断和管理的临床实践指南,我们重点研究了两个类别:确诊 PA(患者表现出明确的生化证据)和边缘 PA(患者表现出边缘生化指标)。在确诊的 PA 病例中,半数以上的患者为 UHA,而约 15% 至 20% 的边缘病例被发现为 UHA。在边缘病例中,低钾血症的发生率被认为是 UHA 的预测因素。在 CT 成像显示无低钾血症和肾上腺结节的边缘病例中,只有 6% 至 8% 的患者被发现患有 UHA。值得注意的是,有些患者在一项检测结果为阴性但另一项检测结果确诊的情况下仍表现出 UHA,尤其是那些 CT 成像显示有低钾血症或肾上腺结节的患者。总之,研究结果验证了 AVS 在确诊 PA 病例中的重要性,以及对边缘病例进行仔细评估的必要性。在可行的情况下,同时进行 CCT 和 SIT,并将其结果与其他临床指标一并解读,可以提供更全面的评估。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Prevalence of unilateral hyperaldosteronism in primary aldosteronism: impact of a novel chemiluminescent immunoassay for measuring plasma aldosterone in Japan
This study aims to evaluate the prevalence of unilateral hyperaldosteronism (UHA) and its clinical characteristics in patients with primary aldosteronism (PA), diagnosed using plasma aldosterone concentration (PAC) measured by chemiluminescent enzyme immunoassay (CLEIA). We retrospectively analyzed data of 199 PA patients from the Japan Primary Aldosteronism Study II (JPAS II) dataset, including patients who underwent adrenal venous sampling (AVS) and the captopril challenge test (CCT) and/or saline infusion test (SIT), with PAC measured by CLEIA. We focused on two categories: confirmed PA, where patients exhibit clear biochemical evidence of the disorder, and borderline PA, where patients present with marginal biochemical indicators, as outlined in the Japan Endocrine Society’s clinical practice guideline for the diagnosis and management of PA. In confirmed PA cases, over the half of patients was UHA, while approximately 15 to 20% of borderline cases were found to be UHA. The prevalence of hypokalemia was identified as predictor of UHA among borderline cases. Among borderline cases with no hypokalemia and adrenal nodules on CT imaging, only 6 to 8% of patients were found to have UHA. Notably, some patients exhibited UHA despite negative results on one test but confirmed result on the other, particularly those with hypokalemia or adrenal nodules on CT imaging. In conclusion, the findings validate the importance of AVS in confirmed PA cases and the need for careful assessment in borderline cases. When feasible, conducting both CCT and SIT, and interpreting their results alongside other clinical indicators, could provide a more comprehensive assessment.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Hypertension Research
医学-外周血管病
CiteScore
7.40
自引率
16.70%
发文量
249
审稿时长
3-8 weeks
期刊介绍:
Hypertension Research is the official publication of the Japanese Society of Hypertension. The journal publishes papers reporting original clinical and experimental research that contribute to the advancement of knowledge in the field of hypertension and related cardiovascular diseases. The journal publishes Review Articles, Articles, Correspondence and Comments.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


