减肥手术中患者和医护人员对患者报告结果的评估--改良德尔菲研究。
IF 4.2
2区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
摘要
背景:患者报告的结果是一个重要的新兴指标,在临床、研究和注册机构中得到越来越多的应用。这些结果虽然非常重要,但却未得到充分利用,需要针对接受减肥手术的特定患者群体加以改进。本研究旨在调查和比较手术前患者、手术后患者和医护人员如何评价患者报告的减肥手术结果,以确定哪些结果被认为是最重要的:方法: 向手术前和手术后的患者以及参与减肥护理的各类医疗从业人员分发了一份改良的德尔菲调查问卷。在两轮调查中,参与者被要求对减肥手术的各种生理和心理结果进行评分,评分范围从 0(不重要)到 10(极其重要)。被至少 70% 的参与者评为 8-10 分的结果被视为非常重要(优先考虑)。结果:20 名手术前患者、95 名手术后患者和 28 名医护人员完成了两轮问卷调查。共有 58 项结果被列为优先事项,其中 21 项结果(共 90 项,占 23.3%)被所有三个小组列为优先事项,13 项(占 14.4%)被两个小组列为优先事项,24 项(占 26.7%)被一个小组或分组列为优先事项。一致优先考虑的结果包括 "并发症"、"一般身体健康"、"总体生活质量 "和 "总体心理健康"。不一致的结果包括 "担心体重增加"、"自杀想法"、"成瘾行为 "和 "羞辱或歧视经历":尽管利益相关者群体对许多结果的看法相当一致,但仍有几项结果的重要性评估不一致,必须加以考虑。特别是,医护人员优先考虑的 20 项结果并不是患者优先考虑的结果,这强调了各利益相关群体优先考虑结果的范围。未来的工作将考虑这些优先级,以确保所产生的测量结果涵盖所有重要结果,并对最终用户有益且有效。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Patient and healthcare practitioner evaluation of patient-reported outcomes in bariatric surgery – a modified Delphi study
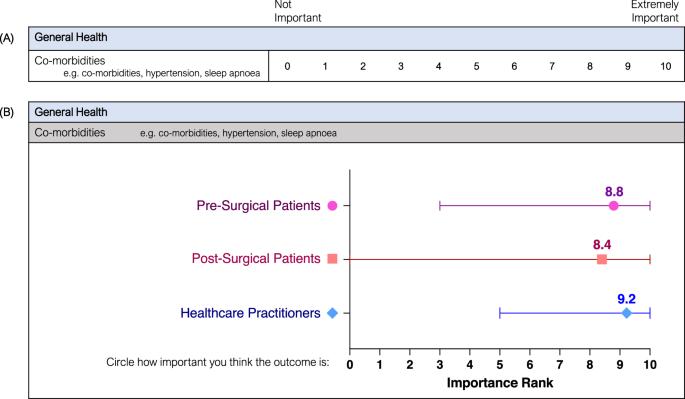
Patient-reported outcomes are an important emerging metric increasingly utilised in clinical, research and registry settings. These outcomes, while vital, are underutilised and require refinement for the specific patient population of those undergoing bariatric surgery. This study aimed to investigate and compare how pre-surgical patients, post-surgical patients, and healthcare practitioners evaluate patient-reported outcomes of bariatric surgery to identify outcomes that are considered most important. A modified Delphi survey was distributed to patients pre- and post-surgery, and to a variety of healthcare practitioners involved in bariatric care. Across two rounds, participants were asked to rate a variety of physical and psychosocial outcomes of bariatric surgery from 0 (Not Important) to 10 (Extremely Important). Outcomes rated 8–10 by at least 70% of participants were considered highly important (prioritised). The highest-rated outcomes were compared between the three groups as well as between medical and allied health practitioner subgroups. 20 pre-surgical patients, 95 post-surgical patients, and 28 healthcare practitioners completed both rounds of the questionnaire. There were 58 outcomes prioritised, with 21 outcomes (out of 90, 23.3%) prioritised by all three groups, 13 (14.4%) by two groups, and 24 (26.7%) prioritised by a single group or subgroup. Unanimously prioritised outcomes included ‘Co-morbidities’, ‘General Physical Health’, ‘Overall Quality of Life’ and ‘Overall Mental Health’. Discordant outcomes included ‘Fear of Weight Regain’, ‘Suicidal Thoughts’, ‘Addictive Behaviours’, and ‘Experience of Stigma or Discrimination’. While there was considerable agreement between stakeholder groups on many outcomes, there remain several outcomes with discordant importance valuations that must be considered. In particular, healthcare practitioners prioritised 20 outcomes that were not prioritised by patients, emphasising the range of priorities across stakeholder groups. Future work will consider these priorities to ensure resulting measures encompass all important outcomes and are beneficial and valid for end users.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

International Journal of Obesity
医学-内分泌学与代谢
CiteScore
10.00
自引率
2.00%
发文量
221
审稿时长
3 months
期刊介绍:
The International Journal of Obesity is a multi-disciplinary forum for research describing basic, clinical and applied studies in biochemistry, physiology, genetics and nutrition, molecular, metabolic, psychological and epidemiological aspects of obesity and related disorders.
We publish a range of content types including original research articles, technical reports, reviews, correspondence and brief communications that elaborate on significant advances in the field and cover topical issues.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


