原发性胆汁性胆管炎患者在任何时候失去生化反应都会使病情恶化
IF 9.5
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
背景& 目的熊去氧胆酸(UDCA)治疗的生化反应与原发性胆汁性胆管炎(PBC)患者的良好预后有关。生化反应通常在疾病早期进行评估,目前尚不清楚有多大比例的患者失去了之前获得的生化反应,也不知道这是否会影响长期无肝移植(LT)生存率。方法我们从加拿大自身免疫性肝病网络中确定了所有接受过 UDCA 治疗的 PBC 患者,并在 1 年时进行了生化测量,评估了他们的肝脏生化随时间变化的情况。生化反应不充分的定义是在 UDCA 治疗 1 年及其后的所有时间点,血清碱性磷酸酶≥正常值上限的 1.67 倍或血清总胆红素异常。多态马尔可夫模型用于估算生化反应状态之间的转换率,以及从每个状态到LT或死亡的转换率。研究结果在外部队列(GLOBAL PBC 登记)中得到验证。诊断时的平均年龄为 53 岁,91% 为女性,33% 的患者在 1 年后对 UDCA 生化反应不足(n = 269)。与随后失去反应的患者相比,最初保持足够反应的患者发生LT或死亡的比例较低(相对比例为0.102,95% CI为0.047-0.223)。与未恢复充分应答的患者(0.016,95% CI 0.001-0.568)和再次失去应答的患者(0.010,95% CI 0.001-0.340)相比,恢复充分应答的患者的比率较低。第三次恢复充分应答的患者的应答率也低于未恢复应答的患者(0.151,95% CI 0.040-0.566)。对全球 PBC 登记(n = 2,237 人)的分析验证了这些结果。影响和意义:对熊去氧胆酸的早期生化反应与原发性胆汁性胆管炎(PBC)患者的良好预后有关。我们的研究表明,随着时间的推移,PBC 患者的生化反应状态会发生转变,而这些转变与肝移植或死亡风险的变化相对应。临床医生应该在整个随访过程中重新评估 PBC 患者的风险并优化治疗决策,无论早期生化治疗反应如何。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Loss of biochemical response at any time worsens outcomes in UDCA-treated patients with primary biliary cholangitis
Background & Aims
Biochemical response to ursodeoxycholic acid (UDCA) therapy is associated with good prognosis in people living with primary biliary cholangitis (PBC). Biochemical response is typically assessed early in disease and it is not known what proportion of patients lose previously attained biochemical response, nor whether this impacts long-term liver transplant (LT)-free survival.
Methods
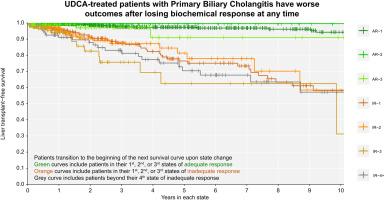
We identified all UDCA-treated patients with PBC from the Canadian Network for Autoimmune Liver disease with biochemical measurements at 1 year, and evaluated their liver biochemistry over time. Inadequate biochemical response was defined as serum alkaline phosphatase ≥1.67x the upper limit of normal or abnormal serum total bilirubin at 1 year of UDCA therapy and all time points thereafter. Multistate Markov models were used to estimate transition rates between biochemical response states and from each state to LT or death. Results were validated in an external cohort (GLOBAL PBC registry).
Results
A total of 823 patients from eight centers were included. Mean age at diagnosis was 53 years, 91% were female, 33% had inadequate biochemical response to UDCA at 1 year (n = 269). Patients who retained initial adequate response had lower rates of LT or death compared to patients who subsequently lost response (relative rate 0.102, 95% CI 0.047-0.223). Patients who regained adequate response had lower rates than patients who did not (0.016, 95% CI 0.001-0.568), and patients who lost response once more (0.010, 95% CI 0.001-0.340). Patients who regained adequate response for a third time also had lower rates than patients who did not (0.151, 95% CI 0.040-0.566). Analyses in the GLOBAL PBC registry (n = 2,237) validated these results.
Conclusion
Loss of biochemical response at any time is associated with heightened risks of LT or death in people living with PBC. Achievement of biochemical response is an important goal throughout follow-up, regardless of biochemical response profile early in therapy.
Impact and implications:
Early biochemical response to ursodeoxycholic acid is associated with good prognosis in patients with primary biliary cholangitis (PBC). Our work demonstrates that patients with PBC transition between biochemical response states over time, and that these transitions correspond with changes in risk of liver transplantation or death. Clinicians should re-evaluate risk and optimize treatment decisions for patients with PBC throughout follow-up, regardless of early biochemical response to therapy.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

JHEP Reports
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
12.40
自引率
2.40%
发文量
161
审稿时长
36 days
期刊介绍:
JHEP Reports is an open access journal that is affiliated with the European Association for the Study of the Liver (EASL). It serves as a companion journal to the highly respected Journal of Hepatology.
The primary objective of JHEP Reports is to publish original papers and reviews that contribute to the advancement of knowledge in the field of liver diseases. The journal covers a wide range of topics, including basic, translational, and clinical research. It also focuses on global issues in hepatology, with particular emphasis on areas such as clinical trials, novel diagnostics, precision medicine and therapeutics, cancer research, cellular and molecular studies, artificial intelligence, microbiome research, epidemiology, and cutting-edge technologies.
In summary, JHEP Reports is dedicated to promoting scientific discoveries and innovations in liver diseases through the publication of high-quality research papers and reviews covering various aspects of hepatology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


