心源性休克和感染:致命的组合
IF 2.3
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
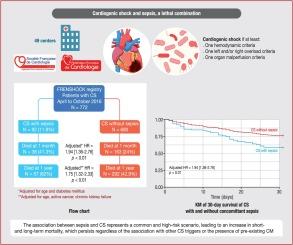
背景心源性休克和脓毒症是严重的血流动力学状态,经常同时出现,导致大量死亡。方法FRENSHOCK是一项前瞻性登记项目,包括来自49个中心的772名心源性休克患者。主要终点是1个月的全因死亡率。结果在纳入的772例心源性休克患者中,有92例由脓毒症引发(占11.9%),表现为更常见的肾脏和肝脏急性损伤,平均动脉压更低。脓毒症组患者需要更广泛地使用多巴酚丁胺(90.1% 对 81.2%;P = 0.16)、去甲肾上腺素(72.5% 对 50.8%;P <;0.01)、肾脏替代疗法(29.7% 对 14%;P <;0.01)、无创通气(36.3% 对 24.4%;P = 0.09)和有创通气(52.7% 对 35.9%;P = 0.02)。脓毒症引发的心源性休克导致较高的1个月(41.3% 对 24.0%;调整后危险比:1.94,95% 置信区间:1.36-2.76;P <;0.01)和1年(62.0% 对 42.9%;调整后危险比:1.75,95% 置信区间:1.32-2.33;P <;0.01)全因死亡率。在心脏移植或心室辅助装置方面,1年后没有发现明显差异(8.7% vs. 10.3%;调整后的几率比0.72,95%置信区间0.32-1.64;P = 0.43)。结论 败血症与心源性休克之间的关联是一种常见的高风险情况,会导致较高的短期和长期死亡率,无论是否与其他心源性休克诱因或是否存在心肌病有关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Cardiogenic shock and infection: A lethal combination
Background
Cardiogenic shock and sepsis are severe haemodynamic states that are frequently present concomitantly, leading to substantial mortality. Despite its frequency and clinical significance, there is a striking lack of literature on the outcomes of combined sepsis and cardiogenic shock.
Methods
FRENSHOCK was a prospective registry including 772 patients with cardiogenic shock from 49 centres. The primary endpoint was 1-month all-cause mortality. Secondary endpoints included heart transplantation, ventricular assistance device and all-cause death rate at 1 year.
Results
Among the 772 patients with cardiogenic shock included, 92 cases were triggered by sepsis (11.9%), displaying more frequent renal and hepatic acute injuries, with lower mean arterial pressure. Patients in the sepsis group required broader use of dobutamine (90.1% vs. 81.2%; P = 0.16), norepinephrine (72.5% vs. 50.8%; P < 0.01), renal replacement therapy (29.7% vs. 14%; P < 0.01), non-invasive ventilation (36.3% vs. 24.4%; P = 0.09) and invasive ventilation (52.7% vs. 35.9%; P = 0.02). Sepsis-triggered cardiogenic shock resulted in higher 1-month (41.3% vs. 24.0%; adjusted hazard ratio: 1.94, 95% confidence interval: 1.36–2.76; P < 0.01) and 1-year (62.0% vs. 42.9%; adjusted hazard ratio 1.75, 95% confidence interval 1.32–2.33; P < 0.01) all-cause death rates. No significant difference was found at 1 year for heart transplantation or ventricular assistance device (8.7% vs. 10.3%; adjusted odds ratio 0.72, 95% confidence interval 0.32–1.64; P = 0.43). In patients with sepsis-triggered cardiogenic shock, neither the presence of a preexisting cardiomyopathy nor the co-occurrence of other cardiogenic shock triggers had any additional impact on death.
Conclusions
The association between sepsis and cardiogenic shock represents a common high-risk scenario, leading to higher short- and long-term death rates, regardless of the association with other cardiogenic shock triggers or the presence of preexisting cardiomyopathy.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Archives of Cardiovascular Diseases
医学-心血管系统
CiteScore
4.40
自引率
6.70%
发文量
87
审稿时长
34 days
期刊介绍:
The Journal publishes original peer-reviewed clinical and research articles, epidemiological studies, new methodological clinical approaches, review articles and editorials. Topics covered include coronary artery and valve diseases, interventional and pediatric cardiology, cardiovascular surgery, cardiomyopathy and heart failure, arrhythmias and stimulation, cardiovascular imaging, vascular medicine and hypertension, epidemiology and risk factors, and large multicenter studies. Archives of Cardiovascular Diseases also publishes abstracts of papers presented at the annual sessions of the Journées Européennes de la Société Française de Cardiologie and the guidelines edited by the French Society of Cardiology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


