EML4-ALK变异和同时出现的TP53突变对ALK酪氨酸激酶抑制剂一线治疗时间和ALK融合阳性NSCLC患者总生存期的影响:来自 GuardantINFORM 数据库的真实世界结果。
IF 21
1区 医学
Q1 ONCOLOGY
引用次数: 0
摘要
简介:酪氨酸激酶抑制剂(TKIs)是ALK阳性(ALK+)非小细胞肺癌(NSCLC)的一线治疗选择。循环肿瘤DNA(ctDNA)中的变异等位基因频率(VAF)、EML4-ALK融合变异和并发TP53突变(TP53mt)等因素可能会影响治疗效果。我们在真实世界中评估了它们对新一代 ALK TKIs 一线治疗停药时间(TTD)的影响:我们在 GuardantINFORM 中确定了接受新一代 ALK TKI 单药一线治疗的晚期/转移性 NSCLC 和 ctDNA 检测到 ALK 融合的成人患者。评估了ALK融合VAF、EML4-ALK变异和TP53mt检测对TTD的影响:基线ctDNA中存在ALK融合的307例患者接受了一线阿来替尼(280例)、布加替尼(15例)、洛拉替尼(9例)或色瑞替尼(3例)治疗;150例患者(49%)的ALK融合VAF≥1%。在232例EML4-ALK融合患者(v1,50%;v3,36%)中,有42例(18%)和32例(14%)TP53mt与v1并发,v3与TP53mt并发。具有 VAF 的患者高ctDNA VAF、EML4-ALK v3和TP53mt与早期停用一线ALK TKIs有关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
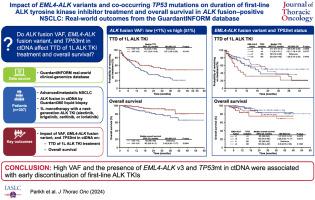
Impact of EML4-ALK Variants and Co-Occurring TP53 Mutations on Duration of First-Line ALK Tyrosine Kinase Inhibitor Treatment and Overall Survival in ALK Fusion-Positive NSCLC: Real-World Outcomes From the GuardantINFORM database
Introduction
Tyrosine kinase inhibitors (TKIs) are first-line treatment options for ALK-positive (ALK+) NSCLC. Factors such as variant allele frequencies (VAFs), EML4-ALK fusion variant, and concurrent TP53 mutations (TP53mt) in circulating tumor DNA (ctDNA) may affect treatment outcomes. We evaluated their effects on time to discontinuation (TTD) of first-line treatment with next-generation ALK TKIs in a real-world setting.
Methods
Adults with advanced or metastatic NSCLC and ctDNA-detected ALK fusion who received first-line next-generation ALK TKI monotherapy were identified in GuardantINFORM. Effects of ALK fusion VAF, EML4-ALK variants, and TP53mt detection on TTD were evaluated.
Results
A total of 307 patients with ALK fusion in baseline ctDNA received first-line alectinib (n = 280), brigatinib (n = 15), lorlatinib (n = 9), or ceritinib (n = 3); 150 patients (49%) had ALK-fusion VAF greater than or equal to 1%. Among 232 patients with EML4-ALK fusions (v1, 50%; v3, 36%), TP53mt co-occurred with v1 in 42 (18%) and v3 in 32 (14%). Patients with VAF less than 1% versus greater than or equal to 1% had a median TTD of 32.2 (95% confidence interval [CI]: 20.7–not estimable [NE]) versus 14.7 months (10.4–19.9; hazard ratio [HR] = 1.57 [95% CI: 1.09–2.26]; p = 0.0146). Median TTD was 13.1 (9.5–19.9) versus 27.6 months (17.3–NE) in patients with versus without TP53mt detected (HR = 1.53 [1.07–2.19]; p = 0.0202) and 20.3 (14.4–NE) versus 11.5 months (7.4–31.1) in patients with v1 versus v3 (HR = 1.29 [0.83–2.01]; p = 0.2641). Patients with TP53mt and v3 had a median TTD of 7.4 months (95% CI: 4.2–31.1).
Conclusion
High ctDNA VAF, EML4-ALK v3, and TP53mt were associated with early discontinuation of first-line ALK TKIs.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Thoracic Oncology
医学-呼吸系统
CiteScore
36.00
自引率
3.90%
发文量
1406
审稿时长
13 days
期刊介绍:
Journal of Thoracic Oncology (JTO), the official journal of the International Association for the Study of Lung Cancer,is the primary educational and informational publication for topics relevant to the prevention, detection, diagnosis, and treatment of all thoracic malignancies.The readship includes epidemiologists, medical oncologists, radiation oncologists, thoracic surgeons, pulmonologists, radiologists, pathologists, nuclear medicine physicians, and research scientists with a special interest in thoracic oncology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


