性别与慢性肾脏病患者罹患动脉粥样硬化性和非动脉粥样硬化性心血管疾病的风险:CKD-REIN 队列研究的发现。
IF 9.4
1区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
摘要
理由和目标:心血管疾病(CVD)的性别差异已得到证实,但慢性肾脏疾病(CKD)是否会改变这些风险差异,以及动脉粥样硬化性心血管疾病(ACVD)和非动脉粥样硬化性心血管疾病(N-ACVD)之间是否存在差异尚不清楚。评估这种相互作用是本研究的主要目标:前瞻性队列研究:2013年至2020年,法国40家肾脏病诊所的全国代表性样本--CKD-肾脏流行病学和信息网络(CKD-REIN)队列中的成年人:致死和非致死的复合 ACVD 事件(缺血性冠心病、脑血管病和外周动脉疾病)和复合 N-ACVD 事件(心力衰竭、出血性中风和心律失常):分析方法:多变量特定病因 Cox 比例危险模型:研究对象包括 1,044 名女性和 1,976 名男性中重度 CKD 患者(中位年龄为 67 岁对 69 岁;平均估计肾小球滤过率[eGFR]为 32±12 对 33±12 mL/min/1.73m2)。在中位随访 5.0(四分位间范围,4.8;5.2)年期间,女性的 ACVD 发生率(每 100 患者年)显著低于男性:2.1(95% 置信区间:1.6-2.5) vs 3.6(3.2-4.0)(P2),并且在较低的 eGFR 水平上逐渐减弱,在 16 mL/min/1.73m2 时达到 1.00(0.62;1.63)。相比之下,在所研究的 eGFR 范围内,N-ACVD 危险在性别间没有差异:局限性:未对心血管生物标志物和性激素进行评估:这项研究表明,女性发生心血管疾病的风险低于男性,但随着肾脏疾病的进展,这种风险会完全减弱。在不同的 CKD 阶段,两性之间发生 N-ACVD 的风险相同,而且其与 eGFR 的关系更为陡峭,这表明 CKD 对这一心血管疾病类型的发展具有重要作用。本文章由计算机程序翻译,如有差异,请以英文原文为准。
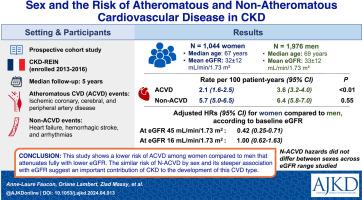
Sex and the Risk of Atheromatous and Nonatheromatous Cardiovascular Disease in CKD: Findings From the CKD-REIN Cohort Study
Rationale & Objective
Sex differences in cardiovascular disease (CVD) are well established, but whether chronic kidney disease (CKD) modifies these risk differences and whether they differ between atheromatous CVD (ACVD) and nonatheromatous CVD (NACVD) is unknown. Assessing this interaction was the principal goal of this study.
Study Design
Prospective cohort study.
Setting & Participants
Adults enrolled in the CKD-REIN (CKD-Renal Epidemiology and Information Network) cohort, a nationally representative sample of 40 nephrology clinics in France, from 2013 to 2020.
Exposure
Sex.
Outcomes
Fatal and nonfatal composite ACVD events (ischemic coronary, cerebral, and peripheral artery disease) and composite NACVD events (heart failure, hemorrhagic stroke, and arrhythmias).
Analytical Approach
Multivariable cause-specific Cox proportional hazards models.
Results
1,044 women and 1,976 men with moderate to severe CKD (median age, 67 vs 69 y; mean estimated glomerular filtration rate [eGFR], 32 ± 12 vs 33 ± 12 mL/min/1.73 m2) were studied. During a median follow-up of 5.0 (IQR, 4.8-5.2) years, the ACVD rate (per 100 patient-years) was significantly lower in women than in men, at 2.1 (95% CI, 1.6-2.5) versus 3.6 (3.2-4.0; P < 0.01), whereas the NACVD rate was not, at 5.7 (5.0-6.5) versus 6.4 (5.8-7.0; P = 0.55). NACVD had a steeper relationship with eGFR than did ACVD. There was an interaction (P < 0.01) between sex and baseline eGFR and the ACVD hazard: the adjusted HR for women versus men was 0.42 (0.25-0.71) at 45 mL/min/1.73 m2 and gradually attenuated at lower levels of eGFR, reaching 1.00 (0.62-1.63) at 16 mL/min/1.73 m2. In contrast, the NACVD hazard did not differ between sexes across the eGFR range studied.
Limitations
Cardiovascular biomarkers and sex hormones were not assessed.
Conclusions
This study shows how the lower risk of ACVD among women versus men attenuates fully with kidney disease progression. The equal risk of NACVD between sexes across CKD stages and its steeper association with eGFR suggest an important contribution of CKD to the development of this CVD type.
Plain-Language Summary
Sex differences in the risks of atheromatous and nonatheromatous cardiovascular disease (CVD) are well established in the general population. If or how chronic kidney disease (CKD) might modify these risks is unknown. In this large cohort of 3,010 patients with CKD, women had a lower risk than men of atheromatous CVDs such as coronary artery disease or stroke when they were at an early stage of CKD. This advantage, partly due to women’s better cardiovascular risk profile, tended to attenuate as CKD progressed to kidney failure. In contrast, the risk of nonatheromatous CVDs such as heart failure for women with CKD appeared similar to that of men with CKD at all kidney function levels.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
American Journal of Kidney Diseases
医学-泌尿学与肾脏学
CiteScore
20.40
自引率
2.30%
发文量
732
审稿时长
3-8 weeks
期刊介绍:
The American Journal of Kidney Diseases (AJKD), the National Kidney Foundation's official journal, is globally recognized for its leadership in clinical nephrology content. Monthly, AJKD publishes original investigations on kidney diseases, hypertension, dialysis therapies, and kidney transplantation. Rigorous peer-review, statistical scrutiny, and a structured format characterize the publication process. Each issue includes case reports unveiling new diseases and potential therapeutic strategies.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


