麦康奈尔征兆可预测急性肺栓塞患者的正常血压休克。
IF 2.5
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
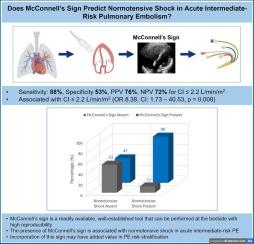
背景:中危肺栓塞(PE)和血压正常休克患者的预后可能较差。然而,正常血压休克的诊断需要有创血液动力学检查。我们的目的是评估麦康奈尔征在识别中危 PE 患者正常血压休克方面的预测价值:研究纳入了 2020 年 8 月至 2023 年 4 月期间在一家大型公立学术医院接受经皮机械血栓切除术的中危 PE 患者。正常血压休克的定义是:收缩压≥90 mmHg,无血管加压支持,术前有创测量心脏指数≤2.2 L/min/m2,临床证据显示灌注不足(即乳酸升高、少尿)。主要结果是麦康奈尔征与正常血压休克之间的关联:结果:有麦康奈尔征的患者(29/40,72.5%)心率较高(114 次/分 vs 99 次/分,p = 0.008),乳酸升高率较高(86% vs 55%,p = 0.038),心脏指数较低(1.9 L/min/m2 vs 3.1 L/min/m2,p = 0.003),正常血压休克率较高(76% vs 27%,p = 0.005)。麦康奈尔征对识别血压正常休克的中危 PE 患者的敏感性为 88%,特异性为 53%。具有麦康奈尔征的患者发生正常血压休克的几率增加(几率比 8.38,置信区间:1.73-40.53,p = 0.008;曲线下面积 0.70,95 % 置信区间:0.56-0.85):这是第一项表明麦康奈尔征可识别中危人群中存在正常血压休克风险的研究。需要更大规模的队列来验证我们的研究结果。本文章由计算机程序翻译,如有差异,请以英文原文为准。
McConnell's sign predicts normotensive shock in patients with acute pulmonary embolism
Background
Patients with intermediate-risk pulmonary embolism (PE) and normotensive shock may have worse outcomes. However, diagnosis of normotensive shock requires invasive hemodynamics. Our objective was to assess the predictive value of McConnell's sign in identifying normotensive shock in patients with intermediate-risk PE.
Methods
Patients with intermediate-risk PE who underwent percutaneous mechanical thrombectomy between August 2020 and April 2023 at a large academic public hospital were included in the study. Normotensive shock was defined as systolic blood pressure ≥ 90 mmHg without vasopressor support with pre-procedural invasive measures of cardiac index ≤2.2 L/min/m2 and clinical evidence of hypoperfusion (i.e. elevated lactate, oliguria). The primary outcome was the association between McConnell's sign and normotensive shock.
Results
Those with McConnell's sign (29/40, 72.5 %) had higher heart rate (114 vs 99 beats/min, p = 0.008), higher rates of elevated lactate (86 % vs 55 %, p = 0.038), lower cardiac index (1.9 vs 3.1 L/min/m2, p = 0.003), and higher rates of normotensive shock (76 % vs 27 %, p = 0.005). McConnell's sign had a sensitivity of 88 % and specificity of 53 % for identifying intermediate-risk PE patients with normotensive shock. Patients with McConnell's sign had an increased odds (odds ratio 8.38, confidence interval: 1.73–40.53, p = 0.008; area under the curve 0.70, 95 % confidence interval: 0.56–0.85) of normotensive shock.
Conclusion
This is the first study to suggest that McConnell's sign may identify those in the intermediate-risk group who are at risk for normotensive shock. Larger cohorts are needed to validate our findings.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of cardiology
CARDIAC & CARDIOVASCULAR SYSTEMS-
CiteScore
4.90
自引率
8.00%
发文量
202
审稿时长
29 days
期刊介绍:
The official journal of the Japanese College of Cardiology is an international, English language, peer-reviewed journal publishing the latest findings in cardiovascular medicine. Journal of Cardiology (JC) aims to publish the highest-quality material covering original basic and clinical research on all aspects of cardiovascular disease. Topics covered include ischemic heart disease, cardiomyopathy, valvular heart disease, vascular disease, hypertension, arrhythmia, congenital heart disease, pharmacological and non-pharmacological treatment, new diagnostic techniques, and cardiovascular imaging. JC also publishes a selection of review articles, clinical trials, short communications, and important messages and letters to the editor.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


