产后月经周期对近期子痫前期妇女体内醛固酮和肾素的不同影响。
IF 2.7
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
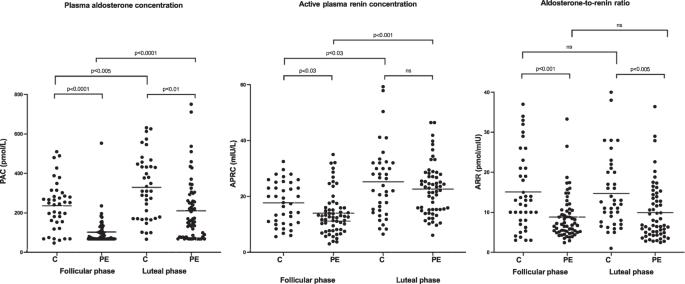
本研究的目的是确定产后月经周期对既往有子痫前期妊娠史和无子痫前期妊娠史妇女的醛固酮、肾素及其比率的影响。为此,我们分析了 59 名有子痫前期病史的妇女和 39 名健康的准对照组妇女的数据。产后五到七个月,我们在月经周期的卵泡期和黄体期测量了醛固酮、肾素以及醛固酮与肾素的比值。所有测量均在早晨仰卧位进行。在测量前一周,患者保持标准钠饮食。我们的研究结果表明,与卵泡期相比,患有近期子痫前期的产后妇女和对照组的肾素和醛固酮平均水平在黄体期明显升高。醛固酮与肾素的比率在两组中均无差异。与对照组相比,患有子痫前期的妇女在卵泡期的肾素、醛固酮和醛固酮-肾素比值水平明显较低。除肾素外,其他指标在黄体期仍保持一致。在对照组中,黄体期和卵泡期醛固酮与肾素的比率之间存在密切的相关性,但在子痫前期组中却不存在这种相关性。我们的结论是,肾素和醛固酮都会受到月经周期的显著影响,而由此产生的醛固酮与肾素的比率则不会。与对照组相比,近期患子痫前期的产后妇女的醛固酮值和醛固酮与肾素的比值往往较低。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Variable effect of the post-partum menstrual cycle on aldosterone and renin in women with recent preeclampsia
The purpose of the present study is to identify the impact of the postpartum menstrual cycle on aldosterone, renin, and their ratio of women with and without a preeclamptic pregnancy in the past. To this end, we analysed the data from 59 women with a history of preeclampsia and 39 healthy parous controls. Five to seven months post-partum, we measured aldosterone, renin, and the aldosterone-to-renin ratio during both the follicular and the luteal phase of the menstrual cycle. All measurements were taken in the supine position in the morning. Patients had maintained a standardized sodium diet in the week prior to the measurements. Our results show that in both post-partum women with recent preeclampsia and controls, average levels of renin and aldosterone are significantly elevated in the luteal phase as compared to the follicular phase. The aldosterone-to-renin ratio does not differ between the two phases in either group. Compared to controls, women with recent preeclampsia have significantly lower levels of renin, aldosterone, and aldosterone-to-renin ratio in the follicular phase. This remained consistent in the luteal phase, except for renin. A close correlation existed between the luteal and follicular aldosterone-to-renin ratio in the control group but not in the preeclampsia group. We conclude that both renin and aldosterone are significantly affected by the menstrual cycle whereas the resulting aldosterone-to-renin ratio is not. Post-partum women with recent preeclampsia tend to have lower values for aldosterone and the aldosterone-to-renin ratio than controls.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


