内镜下黏膜切除术与内镜下黏膜下剥离术治疗巴雷特氏肿瘤和食管腺癌的比较:系统综述与 Meta 分析》(Endoscopic Mucosal Resection versus Endoscopic Submucosal Dissection for Barrett's Neoplasia and Esophageal Adenocarcinoma)。
IF 6.7
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
背景和目的:内镜下粘膜切除术(EMR)和内镜下粘膜下剥离术(ESD)都是治疗巴雷特食管相关肿瘤和食管腺癌(EAC)的公认切除策略。然而,关于哪种技术能提供更好的疗效,目前还缺乏共识。本研究旨在系统回顾在治疗巴雷特瘤和 EAC 时,EMR 与 ESD 的比较证据:我们检索了三个数据库(Embase、MEDLINE、Cochrane Central),直至 2023 年 10 月。我们纳入了比较 EMR 和 ESD 对 Barrett 肿瘤和 EAC 疗效的研究。主要结果包括全切、R0、根治性切除、发育不良完全缓解(CRD)和局部复发。次要结果包括不良事件:我们的搜索发现了 905 条记录。最终分析纳入了 11 项研究。数据显示,ESD的全块切除率明显更高[几率比(OR)=27.36(95% 置信区间(CI):7.12-105.21),p结论:这项系统综述和荟萃分析表明,ESD可实现更高的整块切除率、R0切除率和治愈率,并有降低复发率的趋势。这些结果表明,ESD 可能是治疗巴雷特肿瘤和 EAC 的更有效选择。本文章由计算机程序翻译,如有差异,请以英文原文为准。
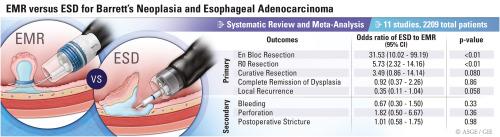
Comparison of EMR versus endoscopic submucosal dissection for Barrett’s neoplasia and esophageal adenocarcinoma: a systematic review and meta-analysis
Background and Aims
EMR and endoscopic submucosal dissection (ESD) are both accepted resection strategies for Barrett’s esophagus–related neoplasia and esophageal adenocarcinoma (EAC). However, a lack of consensus exists regarding which technique offers superior outcomes. This study aims to systematically review the evidence comparing EMR versus ESD in treating Barrett’s neoplasia and EAC.
Methods
We searched 3 databases (Embase, MEDLINE, Cochrane Central) through October 2023. We included studies comparing the efficacy of EMR and ESD for Barrett’s neoplasia and EAC. Primary outcomes include en bloc, R0, and curative resection; complete remission of dysplasia (CRD), and local recurrence. Secondary outcomes encompass adverse events.
Results
Our search identified 905 records. Eleven studies were included in the final analyses. Data showed significantly higher en bloc resection rates with ESD (odds ratio [OR], 31.53; 95% confidence interval [CI], 10.02-99.19; P < .01; 7 studies). R0 resection rates were significantly higher with ESD (OR, 5.92; 95% CI, 2.75-12.77; P < .01; 8 studies). Curative resection rates tended to be higher with ESD (OR, 3.49; 95% CI, 0.86-14.14; P = .080; 4 studies). There was no significant difference in CRD rates (OR, 0.92; 95% CI, 0.37-2.26; P = .86; 3 studies). Local recurrence rates tended to be lower with ESD (OR, 0.35; 95% CI, 0.11-1.04; P = .058; 10 studies). As for adverse events, there was no significant difference in bleeding, perforation, and postoperative stricture rates.
Conclusions
This systematic review and meta-analysis demonstrates that ESD achieves higher en bloc, R0, and curative resection rates, with a tendency toward lower recurrence rates. These results suggest that ESD may be a more effective option for managing Barrett’s neoplasia and EAC. (International Prospective Register of Systematic Reviews [PROSPERO] registration number: CRD42023426486.)
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Gastrointestinal endoscopy
医学-胃肠肝病学
CiteScore
10.30
自引率
7.80%
发文量
1441
审稿时长
38 days
期刊介绍:
Gastrointestinal Endoscopy is a journal publishing original, peer-reviewed articles on endoscopic procedures for studying, diagnosing, and treating digestive diseases. It covers outcomes research, prospective studies, and controlled trials of new endoscopic instruments and treatment methods. The online features include full-text articles, video and audio clips, and MEDLINE links. The journal serves as an international forum for the latest developments in the specialty, offering challenging reports from authorities worldwide. It also publishes abstracts of significant articles from other clinical publications, accompanied by expert commentaries.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


