妇女心血管代谢疾病与体重之间的关系:哪些途径会增加患糖尿病和心血管疾病的风险?
IF 3.4
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
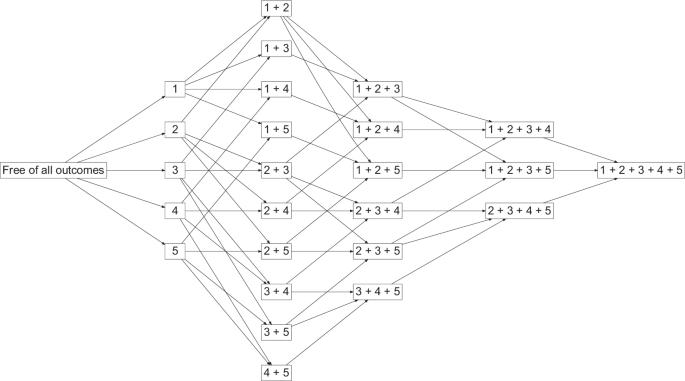
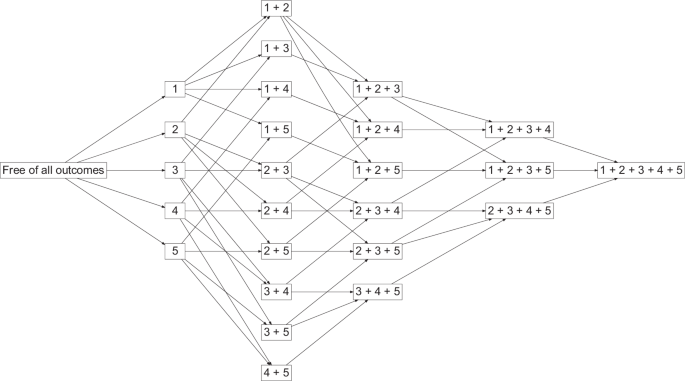
以往的研究调查了体重和高血压与心血管代谢多病发病风险的关系。我们的目的是估算中年时期超重、肥胖和高血压不同发展模式的受试者日后罹患糖尿病和心血管疾病的风险。这是一项前瞻性队列研究,使用了澳大利亚妇女健康纵向研究(Australian Longitudinal Study on Women's Health)中 12784 名参与者的数据。研究采用了多州模型来研究超重、肥胖、高血压、糖尿病和心血管疾病在生命过程中的发展模式。对患有其他疾病的不同模式的妇女在 73 岁之前的糖尿病和心血管疾病累积发病率进行了估算。六种最常见的糖尿病发病途径和相应的累积发病率分别是:超重 5.1%、肥胖 11.5%、高血压 6.9%、从超重发展到肥胖 8.2%、超重和高血压 12.1%、肥胖和高血压 36.8%。对于患有糖尿病和其他疾病的妇女来说,心血管疾病(心脏病或中风)的累积发病率为 22.4%。仅报告有糖尿病但没有高体重或高血压的妇女的相应数字为 8.3%。从健康状态转变为心脏代谢疾病的风险较高与教育程度低、收入压力大、吸烟、不饮酒(与低度饮酒者相比)、缺乏运动和感知压力大有关。中年肥胖和高血压妇女患糖尿病和心血管疾病的风险大大高于没有这些潜在可预防疾病的妇女。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Transition between cardiometabolic conditions and body weight among women: which paths increase the risk of diabetes and cardiovascular diseases?
Previous studies investigated the association of body weight and hypertension with risk of incident cardiometabolic multimorbidity. Our aim was to estimate the risk of diabetes and cardiovascular disease later in life for subjects with different progression patterns of overweight, obesity, and hypertension in mid-life. This was a prospective cohort study in which data from 12,784 participants in the Australian Longitudinal Study on Women’s Health were used. Multistate model was used to study the progression pattern of overweight, obesity, hypertension, diabetes, and cardiovascular disease over the life course. The cumulative incidence of diabetes and cardiovascular disease up to the age of 73 was estimated for women with different patterns of other conditions. The six most common paths and corresponding cumulative incidences for diabetes were overweight 5.1%, obesity 11.5%, hypertension 6.9%, progression from overweight to obesity 8.2%, overweight and hypertension 12.1%, and obesity and hypertension 36.8%. For women with diabetes and other conditions, the cumulative incidence of cardiovascular disease (heart disease or stroke) as the next immediate condition was 22.4%. The corresponding figure for women who only had a report of diabetes but did not have high body weight or hypertension was 8.3%. The higher risk of transition from healthy state to a cardiometabolic condition was associated with low education, income stress, smoking, not drinking alcohol (compared to low drinkers), physical inactivity, and high perceived stress. Women with obesity and hypertension in middle-age had a substantially higher risk of developing diabetes and cardiovascular disease than women without these potentially preventable conditions.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


