阿尔茨海默病血液生物标志物:人群使用的注意事项
IF 28.2
1区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
摘要
在过去的 5 年中,我们见证了首例获批的阿尔茨海默病(AD)疾病改变疗法,也见证了血液生物标志物(BBM)的发展,以帮助诊断阿尔茨海默病。与腰椎穿刺(采集脑脊液)或神经影像学检查相比,基于血液的生物标记物因其可及性、侵入性和成本等诸多原因,更容易被患者接受,也更可行。然而,在人群中如何更好地使用 BBM 仍存在许多问题。在本综述中,我们将概述在广泛实施和解释 AD BBM 时需要考虑的因素。首先,我们回顾了目前在 AD 中使用生物标记物(包括 BBMs)的情况。我们接着描述了典型的初级医疗认知障碍患者的特征,他们通常不同于 AD BBM 研究中使用的患者群体。我们还考虑了可能影响 BBM 检验解释的因素,如合并症、性别、种族或民族。最后,我们讨论了更广泛的问题,如伦理、患者和医疗服务提供者的偏好、偶然发现、处理不确定的结果以及在人群层面实施 BBM 时的不完全准确性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
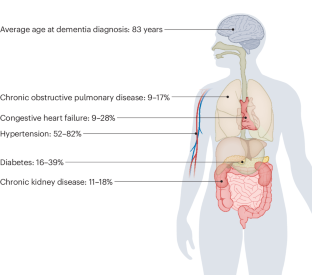
Alzheimer disease blood biomarkers: considerations for population-level use
In the past 5 years, we have witnessed the first approved Alzheimer disease (AD) disease-modifying therapy and the development of blood-based biomarkers (BBMs) to aid the diagnosis of AD. For many reasons, including accessibility, invasiveness and cost, BBMs are more acceptable and feasible for patients than a lumbar puncture (for cerebrospinal fluid collection) or neuroimaging. However, many questions remain regarding how best to utilize BBMs at the population level. In this Review, we outline the factors that warrant consideration for the widespread implementation and interpretation of AD BBMs. To set the scene, we review the current use of biomarkers, including BBMs, in AD. We go on to describe the characteristics of typical patients with cognitive impairment in primary care, who often differ from the patient populations used in AD BBM research studies. We also consider factors that might affect the interpretation of BBM tests, such as comorbidities, sex and race or ethnicity. We conclude by discussing broader issues such as ethics, patient and provider preference, incidental findings and dealing with indeterminate results and imperfect accuracy in implementing BBMs at the population level. Blood-based biomarkers have the potential to transform the Alzheimer disease diagnostic pathway, but many questions remain regarding their implementation and utilization. This Review considers factors that might affect the interpretation of blood-based biomarker tests, including comorbidities, sex and race or ethnicity, and discusses broader issues surrounding their use at the population level.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Nature Reviews Neurology
医学-临床神经学
CiteScore
29.90
自引率
0.80%
发文量
138
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Neurology aims to be the premier source of reviews and commentaries for the scientific and clinical communities we serve. We want to provide an unparalleled service to authors, referees, and readers, and we work hard to maximize the usefulness and impact of each article. The journal publishes Research Highlights, Comments, News & Views, Reviews, Consensus Statements, and Perspectives relevant to researchers and clinicians working in the field of neurology. Our broad scope ensures that the work we publish reaches the widest possible audience. Our articles are authoritative, accessible, and enhanced with clearly understandable figures, tables, and other display items. This page gives more detail about the aims and scope of the journal.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


