强直性脊柱炎患者在白细胞介素17抑制剂治疗期间的葡萄膜炎病程
摘要
生物改良抗风湿药(bDMARDs)对强直性脊柱炎(AS)的各种临床表现有不同的影响。有关白细胞介素17抑制剂(IL17-i)对强直性脊柱炎葡萄膜炎影响的数据仍在不断积累。目的:评估IL17-i疗法对强直性脊柱炎葡萄膜炎病程的影响。研究涉及73名强直性脊柱炎患者(纽约标准,1984年),他们接受IL17-i(57-secukinumab (SEC),22-netakimab (NTK))治疗至少1年。患者纳入研究时的平均年龄为(41.93±8.95)岁,强直性脊柱炎的平均病程为(10.75±6.22)年。患者中有 40 名男性(56.7%)和 33 名女性(43.3%)。62/73(85%)例患者检测到 HLA-B27,58(79%)例患者患有髋关节炎,63(86.3%)例患者患有腱鞘炎,57(78%)例患者患有外周关节炎,7(9.5%)例患者患有银屑病,3(4.1%)例患者患有炎症性肠病(IBD);6(8.2%)例患者在 16 岁前开始患病;19(26%)例患者在患病期间至少发作过一次葡萄膜炎。葡萄膜炎的发病率是通过比较开始使用 bDMARDs 治疗前和使用 IL17-i 期间每 100 患者年的发病次数估算得出的。在开始使用bDMARDs治疗前,所有患者的葡萄膜炎发病率为每100 pt-年8.3例(95% CI 0.065-0.107),在使用IL17-i治疗期间为每100 pt-年9.2例(95% CI 0.06-0.15),P = 0.72。在开始使用bDMARDs治疗前,使用SEC的患者葡萄膜炎发病率为每100 pt-年10.1例(95% CI 0.079-0.13),在SEC治疗期间为每100 pt-年9.4例(95% CI 0.05-0.15),P = 0.74。使用NTK的患者葡萄膜炎发病率在开始使用bDMARDs治疗前为每100 pt-年4.8例(95% CI 0.028-0.08),在NTK治疗期间为每100 pt-年7.1例(95% CI 0.019-022),p = 0.3。对于有葡萄膜炎病史的患者,在开始使用bDMARDs治疗前,葡萄膜炎的发生率为每100 pt-年22.5例(95% CI 0.18-0.28),在IL17-i治疗期间,葡萄膜炎的发生率为每100 pt-年29.1例(95% CI 0.18-0.43),p = 0.29。在 SEC 治疗期间,57 例患者中有 4 例(7%)出现葡萄膜炎;在 NTK 治疗期间,25 例患者中有 1 例(4%)出现葡萄膜炎。在使用 SEC 治疗期间,记录到一例新发葡萄膜炎。与非生物疗法相比,IL17-i疗法的葡萄膜炎发病率没有明显差异。在研究组中,IL17-i疗法对强直性脊柱炎葡萄膜炎的病程没有明显影响。
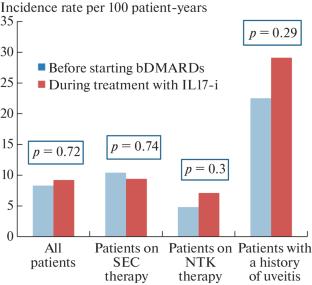

Biological disease-modifying antirheumatic drugs (bDMARDs) can have different effects on various clinical manifestations of ankylosing spondylitis (AS). Data on the effects of interleukin 17 inhibitors (IL17-i) on uveitis in AS continue to accumulate. Objective: to evaluate the effect of IL17-i therapy on the course of uveitis in AS. The study involved 73 patients with AS (New York criteria, 1984), who received IL17-i (57—secukinumab (SEC), 22—netakimab (NTK)) for at least 1 year. The average age of patients at the time of inclusion in the study was 41.93 ± 8.95 years, the average duration of AS was 10.75 ± 6.22 years. There were 40 men (56.7%) and 33 women (43.3%) among the patients. HLA-B27 was detected in 62/73 (85%), coxitis in 58 (79%), enthesitis in 63 (86.3%), peripheral arthritis in 57 (78%), psoriasis in 7 (9.5%), and inflammatory bowel disease (IBD) in 3 (4.1%) patients; in 6 (8.2%) patients, the disease started before the age of 16; 19 (26%) patients had at least one episode of uveitis during the course of the disease. The rates of uveitis was estimated by comparing the number of incidences per 100 patient-years before the start of bDMARDs therapy and during IL17-i using. The incidence rate of uveitis before the start of bDMARDs therapy for all patients was 8.3 per 100 pt-years (95% CI 0.065–0.107), during IL17-i therapy— 9.2 per 100 pt-years (95% CI 0.06–0.15), p = 0.72. The incidence rate of uveitis among patients who used SEC was 10.1 per 100 pt-years (95% CI 0.079–0.13) before the start of bDMARDs therapy and 9.4 per 100 pt-years (95% CI 0.05-0.15), p = 0.74 during SEC therapy. The incidence rate of uveitis among patients who used NTK was 4.8 per 100 pt-years (95% CI 0.028–0.08) before the start of bDMARDs therapy and 7.1 per 100 pt-years (95% CI 0.019–022), p = 0.3 during the NTK therapy. For patients with a history of uveitis, the incidence rate of uveitis was 22.5 per 100 pt-years (95% CI 0.18–0.28) before the start of therapy with bDMARDs and 29.1 per 100 pt-years (95% CI 0.18–0.43), p = 0.29 during IL17-i therapy. Occurrences of uveitis were observed in 4 of 57 patients (7%) during SEC therapy and in 1 of 25 (4%) patients during the NTK therapy. One case of new-onset uveitis was recorded during the using of SEC. There were no significant differences in the incidence rates of uveitis during IL17-i therapy compared with non-biological therapy. IL17-i therapy have not demonstrated a significant effect on the course of uveitis in AS in the study group.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


