内镜下切除锯齿状息肉后罹患远期结直肠癌或晚期病变的风险因素:系统综述和荟萃分析。
IF 6.7
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
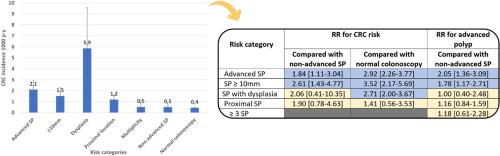
背景和目的:有锯齿状息肉 (SP) 是 15-20% 大肠癌 (CRC) 的前兆。然而,关于哪些SP需要监测以及监测的时间间隔还存在不确定性,在缺乏确凿证据的情况下,我们根据腺瘤的监测建议进行了调整。我们的目的是评估哪些 SP 风险特征与罹患晚期 CRC 或晚期息肉的较高风险有关:我们系统地检索了 PubMed、EMBASE 和 Cochrane 中从开始到 2023 年 12 月 31 日的队列、病例对照研究和临床试验,以了解按基线 SP 大小、发育不良、位置和多发性分层监测的 CRC 或晚期息肉 [晚期腺瘤 (AA) 或晚期 SP] 发生率。我们将晚期息肉定义为大于 10 毫米或发育不良的息肉。我们估算了每千人年的 CRC 和晚期息肉发病率(p-y)。我们采用随机效应模型计算了汇总相对风险(RR),从而进行了荟萃分析:共审查了 5903 项研究,纳入了 14 项研究,共有 493949 名患者(平均年龄 59-5 岁,55% 为男性)。平均随访时间为 4-9 年。晚期SP每1,000 p-y的CRC发病率为2-09(95%CI为1-29-2-90),SP>10mm为1-52(0-78-2-25),SP伴发育不良为5-86(2-16-9-56),近端SP为1-18(0-77-1-60),>3SP为0-52(0-08-1-12),非晚期SP为0-50(0-35-0-66),结肠镜检查正常为0-44(0-41-0-46)。结论:基线晚期 SP 患者在随访 4-9 年后患 CRC 的风险明显升高,其风险大小与 AA 患者的风险大小相似,支持目前对晚期 SP 患者进行 3 年监测的建议。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Risk factors for metachronous colorectal cancer or advanced lesions after endoscopic resection of serrated polyps: a systematic review and meta-analysis
Background and Aims
Serrated polyps (SPs) are precursors to 15% to 20% of colorectal cancers (CRCs). However, there are uncertainties regarding which SPs require surveillance and at what intervals, with recommendations adapted from those for adenomas in the absence of solid evidence. Our aim was to assess which SP risk characteristics relate to a higher risk of metachronous CRC or advanced polyps.
Methods
We systematically searched PubMed, Embase, and Cochrane for cohort studies, case-control studies, and clinical trials from inception to December 31, 2023, of CRC or advanced polyps (advanced adenoma [AA] or advanced SP) incidence at surveillance stratified by baseline SP size, dysplasia, location, and multiplicity. We defined advanced SPs as those ≥10 mm or with dysplasia. CRC and advanced polyp incidence per 1000 person-years were estimated. We performed a meta-analysis by calculating pooled relative risks (RRs) using a random-effects model.
Results
A total of 5903 studies were reviewed, and 14 were included with 493,949 patients (mean age, 59.5 years; 55% men). The mean follow-up was 4.9 years. CRC incidence per 1000 person-years was 2.09 (95% confidence interval [CI], 1.29-2.90) for advanced SPs, 1.52 (95% CI, 0.78-2.25) for SPs of ≥10 mm, 5.86 (95% CI, 2.16-9.56) for SPs with dysplasia, 1.18 (95% CI, 0.77-1.60) for proximal SPs, 0.52 (95% CI, 0.08-1.12) for ≥3 SPs, 0.50 (95% CI, 0.35-0.66) for nonadvanced SPs, and 0.44 (95% CI, 0.41-0.46) for normal colonoscopy findings. Metachronous CRC risk was higher in advanced SPs versus nonadvanced SPs (RR, 1.84; 95% CI, 1.11-3.04) and versus normal colonoscopy findings (RR, 2.92; 95% CI, 2.26-3.77), in SPs of ≥10 mm versus <10 mm (RR, 2.61; 95% CI, 1.43-4.77) and versus normal colonoscopy findings (RR: 3.52; 95% CI, 2.17-5.69); and in SPs with dysplasia versus normal colonoscopy findings (RR: 2.71; 95% CI, 2.00-3.67). No increase in CRC or advanced polyp risk was found in patients with proximal versus distal SPs, nor in ≥3 SPs versus 1 or 2 SPs.
Conclusions
CRC risk is significantly higher in patients with baseline advanced SPs after 4.9 years of follow-up, with risk magnitudes similar to those described for AA, supporting the current recommendation for 3-year surveillance in patients with advanced SPs.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Gastrointestinal endoscopy
医学-胃肠肝病学
CiteScore
10.30
自引率
7.80%
发文量
1441
审稿时长
38 days
期刊介绍:
Gastrointestinal Endoscopy is a journal publishing original, peer-reviewed articles on endoscopic procedures for studying, diagnosing, and treating digestive diseases. It covers outcomes research, prospective studies, and controlled trials of new endoscopic instruments and treatment methods. The online features include full-text articles, video and audio clips, and MEDLINE links. The journal serves as an international forum for the latest developments in the specialty, offering challenging reports from authorities worldwide. It also publishes abstracts of significant articles from other clinical publications, accompanied by expert commentaries.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


