1300万青少年在COVID-19后的心理健康困扰:电子健康记录的回顾性队列研究》。
IF 9.2
1区 医学
Q1 PEDIATRICS
Journal of the American Academy of Child and Adolescent Psychiatry
Pub Date : 2025-01-01
DOI:10.1016/j.jaac.2024.03.023
引用次数: 0
摘要
目的:研究 SARS-CoV-2 感染对青少年精神障碍发病率的影响:调查 SARS-CoV-2 感染对青少年精神障碍发病率的影响:研究涉及 TriNetX 研究网络中的 7,519,465 名儿童和 5,338,496 名青少年,他们均无精神障碍病史。其中有 290,145 名儿童和 223,667 名青少年的 SARS-CoV-2 检测结果呈阳性或确诊为 COVID-19。我们利用卡普兰-梅耶尔生存分析法评估了感染后两年内出现新精神障碍(ICD-10-CM F01-F99 类别中的任何代码和自杀行为)的概率,并与倾向得分匹配的未感染青少年进行了比较:结果发现:在感染 SARS-CoV-2 后两年内,儿童获得新的精神疾病诊断的概率为 0.15,而与之匹配的未感染儿童的概率为 0.026;青少年获得新的精神疾病诊断的概率为 0.19,而与之匹配的未感染青少年的概率为 0.05。儿童的危险比(HR)为 6.0(95% 置信区间:5.8-6.3),青少年为 4.2(95% 置信区间:4.1-4.4),儿童与青少年的危险比为 1.4(95% 置信区间:1.36-1.51)。在几乎所有精神障碍和自杀行为的子类别中都观察到了升高的HRs,并因性别、SARS-CoV-2感染的严重程度和病毒变异而有所不同。在增加青少年精神障碍发病率方面,COVID-19 与其他呼吸道感染相似,但对儿童的影响明显更大(HR 1.57,95%CI:1.53-1.61):我们的研究显示,青少年感染 SARS-CoV-2 后会出现严重的心理健康问题,其中儿童比青少年更为明显。这些发现强调了为高危青少年提供支持的紧迫性,尤其是那些感染 SARS-CoV-2 的年龄更小、感染更严重的青少年。本文章由计算机程序翻译,如有差异,请以英文原文为准。
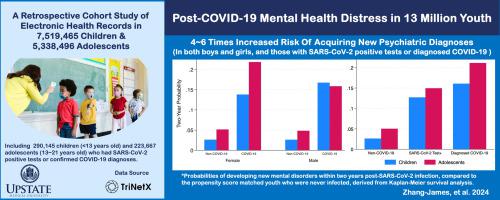
Post–COVID-19 Mental Health Distress in 13 Million Youth: A Retrospective Cohort Study of Electronic Health Records
Objective
To investigate the impact of the SARS-CoV-2 infection on the rates of mental disorders in youth.
Method
The study involved 7,519,465 children and 5,338,496 adolescents from the TriNetX Research Network, all without prior mental disorder histories. Among them, 290,145 children and 223,667 adolescents had SARS-CoV-2–positive tests or confirmed COVID-19 diagnoses. Kaplan–Meier survival analysis was used to evaluate the probability of developing new mental disorders (any codes in International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) F01-F99 category and suicidal behaviors) within 2 years post infection, compared to the propensity score–matched youth who were never infected.
Results
Within 2 years post SARS-CoV-2 infection, children had a probability of 0.15 in acquiring new psychiatric diagnoses, compared to 0.026 for matched non-infected children; adolescents had a 0.19 probability against 0.05 for their non-infected counterparts. The hazard ratio (HR) was 6.0 (95% CI = 5.8-6.3) for children and 4.2 for adolescents (95% CI = 4.1-4.4), with children vs adolescents HR of 1.4 (95% CI = 1.36-1.51). Elevated HRs were observed for almost all subcategories of mental disorders and suicidal behaviors, with variations based on sex, severity of SARS-CoV-2 infection, and viral variants. COVID-19 was similar to other respiratory infections and was associated with a similarly increased rate of mental disorders in adolescents, but had a significantly higher effect on children (HR = 1.57, 95% CI =1.53-1.61).
Conclusion
This study revealed significant mental health distress following SARS-CoV-2 infection in youth, which was more pronounced in children than in adolescents. These findings underscore the urgent need to support at-risk youth, particularly those who contracted SARS-CoV-2 at younger ages and had more severe infections.
Plain language summary
The authors of this study conducted analyses using electronic medical records from the TriNetX Research Network to investigate the impact of SARS-CoV-2 infection on the rates of mental health disorders in youth. Within 2 years after SARS-CoV-2 infection, children and adolescents were 6.0 and 4.2 times more likely to acquire a new psychiatric diagnosis, respectively. While the risk of being diagnosed with a mental health disorder following SARS-CoV-2 infection in adolescents was comparable to other respiratory infections, it had a more pronounced effect on children.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
21.00
自引率
1.50%
发文量
1383
审稿时长
53 days
期刊介绍:
The Journal of the American Academy of Child & Adolescent Psychiatry (JAACAP) is dedicated to advancing the field of child and adolescent psychiatry through the publication of original research and papers of theoretical, scientific, and clinical significance. Our primary focus is on the mental health of children, adolescents, and families.
We welcome unpublished manuscripts that explore various perspectives, ranging from genetic, epidemiological, neurobiological, and psychopathological research, to cognitive, behavioral, psychodynamic, and other psychotherapeutic investigations. We also encourage submissions that delve into parent-child, interpersonal, and family research, as well as clinical and empirical studies conducted in inpatient, outpatient, consultation-liaison, and school-based settings.
In addition to publishing research, we aim to promote the well-being of children and families by featuring scholarly papers on topics such as health policy, legislation, advocacy, culture, society, and service provision in relation to mental health.
At JAACAP, we strive to foster collaboration and dialogue among researchers, clinicians, and policy-makers in order to enhance our understanding and approach to child and adolescent mental health.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


