良性前列腺增生手术相关尿道狭窄的发生率和处理:美国大型数据库的结果。
IF 5.1
2区 医学
Q1 ONCOLOGY
引用次数: 0
摘要
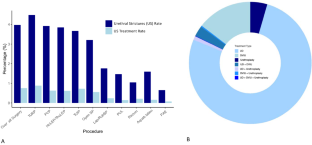
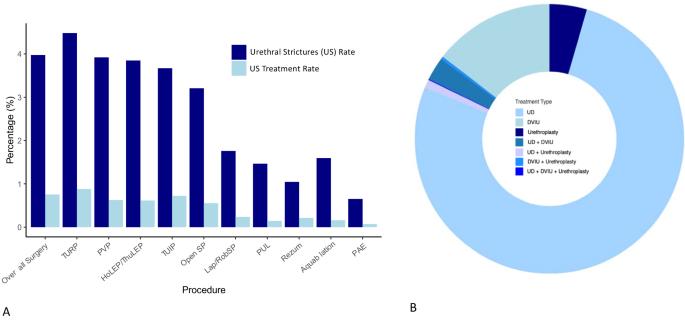
简介和目的:尿道狭窄(US)是良性前列腺增生症(BPH)手术治疗后的一种众所周知的并发症。本研究旨在评估不同类型良性前列腺增生手术后尿道狭窄的当代发生率,确定相关风险因素并评估其处理方法:研究使用 PearlDiver™ Mariner 数据库进行了回顾性分析,该数据库包含 2011 年至 2022 年间编制的去身份化患者记录。采用特定的《国际疾病分类》(ICD)和《现行手术术语》(CPT)代码来确定人群特征和结果。所有治疗良性前列腺增生症最常用的手术方法均在考虑之列。采用多变量逻辑回归评估与术后US诊断相关的因素:结果:在接受良性前列腺增生手术的 274 808 名患者中,有 10 918 名患者(3.97%)在 12 个月内出现了术后 US。TURP(4.48%)、经尿道前列腺切开术(TUIP)(3.67%)、光选择性前列腺汽化术(PVP)(3.92%)、HoLEP/ThuLEP(3.85%)和开放式单纯前列腺切除术(SP)(3.21%)术后出现尿路刺激症状的比例较高。腹腔镜/机器人辅助SP(1.76%)、Aquablation(1.59%)、前列腺尿道提升术(PUL)(1.07%)、Rezum(1.05%)和前列腺动脉栓塞术(PAE)(0.65%)的发病率较低。多变量分析显示,与 TURP 相比,接受 PUL、Rezum、Aquablation、PAE 和 PVP 治疗的患者发生 US 的可能性更低。18.95%的患者需要对尿道扩张进行手术治疗,其中14.55%和4.50%的患者需要进行直视内尿道切开术(DVIU)和尿道成形术。大多数病例(76.7%)的主要治疗方法是在门诊进行尿道扩张术(UD):本研究对当代大型数据集的分析表明,良性前列腺增生症手术后尿道扩张的发生率相对较低 (本文章由计算机程序翻译,如有差异,请以英文原文为准。
Incidence and management of BPH surgery-related urethral stricture: results from a large U.S. database
Urethral stricture (US) is a well-known complication after surgical treatment of benign prostatic hyperplasia (BPH). This study aimed to evaluate the contemporary incidence of the US after different types of BPH surgery, to identify associated risk factors and to assess its management. A retrospective analysis was conducted using the PearlDiver™ Mariner database, containing de-identified patient records compiled between 2011 and 2022. Specific International Classification of Diseases (ICD) and Current Procedural Terminology (CPT) codes were employed to identify population characteristics and outcomes. All the most employed surgical procedures for BPH treatment were considered. Multivariable logistic regression was employed to evaluate factors associated with diagnosis of post-operative US. Among 274,808 patients who underwent BPH surgery, 10,918 developed post-operative US (3.97%) within 12 months. Higher incidence of US was observed following TURP (4.48%), Transurethral Incision of the Prostate (TUIP) (3.67%), Photoselective Vaporization of the Prostate (PVP) (3.92%), HoLEP/ThuLEP (3.85%), and open Simple Prostatectomy (SP) (3.21%). Lower incidence rates were observed after laparoscopic\robot-assisted SP (1.76%), Aquablation (1.59%), Prostatic Urethral Lift (PUL) (1.07%), Rezum (1.05%), and Prostatic Artery Embolization (PAE) (0.65%). Multivariable analysis showed that patients undergoing PUL, Rezum, Aquablation, PAE, and PVP were associated with a reduced likelihood of developing US compared to TURP. US required surgical treatment in 18.95% of patients, with direct visual internal urethrotomy (DVIU) and urethroplasty performed in 14.55% and 4.50% of cases, respectively. Urethral dilatation (UD) in an outpatient setting was the primary management in most cases (76.7%). The present analysis from a contemporary large dataset suggests that the incidence of US after BPH surgery is relatively low (<5%) and varies among procedures. Around 94% of US cases following BPH surgery are managed using minimally invasive treatment approaches such as UD and DVIU.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Prostate Cancer and Prostatic Diseases
医学-泌尿学与肾脏学
CiteScore
10.00
自引率
6.20%
发文量
142
审稿时长
6-12 weeks
期刊介绍:
Prostate Cancer and Prostatic Diseases covers all aspects of prostatic diseases, in particular prostate cancer, the subject of intensive basic and clinical research world-wide. The journal also reports on exciting new developments being made in diagnosis, surgery, radiotherapy, drug discovery and medical management.
Prostate Cancer and Prostatic Diseases is of interest to surgeons, oncologists and clinicians treating patients and to those involved in research into diseases of the prostate. The journal covers the three main areas - prostate cancer, male LUTS and prostatitis.
Prostate Cancer and Prostatic Diseases publishes original research articles, reviews, topical comment and critical appraisals of scientific meetings and the latest books. The journal also contains a calendar of forthcoming scientific meetings. The Editors and a distinguished Editorial Board ensure that submitted articles receive fast and efficient attention and are refereed to the highest possible scientific standard. A fast track system is available for topical articles of particular significance.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


