精氨酸加压素缺乏症:诊断、管理和催产素缺乏症的相关性
IF 31
1区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
摘要
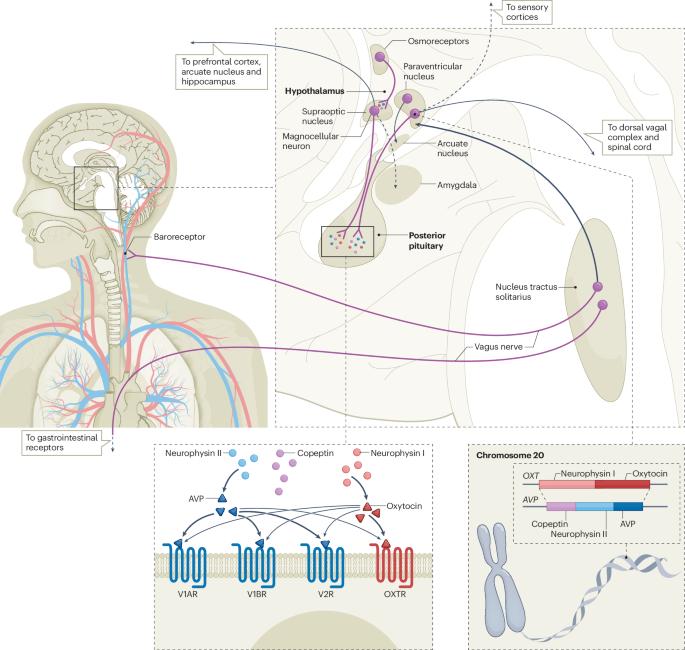
多尿多饮综合征可由中枢性糖尿病性尿崩症、肾源性糖尿病性尿崩症或原发性多尿引起。为了避免与糖尿病混淆,"中枢性糖尿病性尿崩症 "在 2022 年被改名为精氨酸血管加压素(AVP)缺乏症,而 "肾源性糖尿病性尿崩症 "则被改名为 AVP 抵抗症。为了区分这三种类型,过去十年间推出了各种基于渗透性和非渗透性 copeptin 的刺激试验。高渗盐水试验加血浆 copeptin 测量成为诊断准确性最高的试验,取代了缺水试验,成为鉴别诊断多尿多饮综合征的金标准。治疗 AVP 缺乏症的主要方法是用去氨加压素替代 AVP,去氨加压素是 AVP 受体 2(AVPR2)特异性的 AVP 合成类似物,通常能迅速改善多尿和多脂症状。去氨加压素的主要不良反应是稀释性低钠血症,定期使用所谓的去氨加压素逃逸法可以减少这种不良反应。过去几年的证据表明,AVP 缺乏症患者还存在催产素缺乏症。未来的研究应进一步评估这种潜在的不足,包括临床实践中可行的激发试验和催产素替代物的干预试验。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Arginine vasopressin deficiency: diagnosis, management and the relevance of oxytocin deficiency
Polyuria–polydipsia syndrome can be caused by central diabetes insipidus, nephrogenic diabetes insipidus or primary polydipsia. To avoid confusion with diabetes mellitus, the name ‘central diabetes insipidus’ was changed in 2022 to arginine vasopressin (AVP) deficiency and ‘nephrogenic diabetes insipidus’ was renamed as AVP resistance. To differentiate the three entities, various osmotic and non-osmotic copeptin-based stimulation tests have been introduced in the past decade. The hypertonic saline test plus plasma copeptin measurement emerged as the test with highest diagnostic accuracy, replacing the water deprivation test as the gold standard in differential diagnosis of the polyuria–polydipsia syndrome. The mainstay of treatment for AVP deficiency is AVP replacement with desmopressin, a synthetic analogue of AVP specific for AVP receptor 2 (AVPR2), which usually leads to rapid improvements in polyuria and polydipsia. The main adverse effect of desmopressin is dilutional hyponatraemia, which can be reduced by regularly performing the so-called desmopressin escape method. Evidence from the past few years suggests an additional oxytocin deficiency in patients with AVP deficiency. This potential deficiency should be further evaluated in future studies, including feasible provocation tests for clinical practice and interventional trials with oxytocin substitution. Central diabetes insipidus has been renamed as arginine vasopressin deficiency. This Review discusses advances in diagnosis and management of arginine vasopressin deficiency. In addition, the possibility of oxytocin deficiency in these patients is considered, as well as oxytocin provocation testing and the future therapeutic potential of oxytocin replacement.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Nature Reviews Endocrinology
医学-内分泌学与代谢
CiteScore
42.00
自引率
0.70%
发文量
158
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Endocrinology aspires to be the foremost platform for reviews and commentaries catering to the scientific communities it serves. The journal aims to publish articles characterized by authority, accessibility, and clarity, enhanced with easily understandable figures, tables, and other visual aids. The goal is to offer an unparalleled service to authors, referees, and readers, striving to maximize the usefulness and impact of each article. Nature Reviews Endocrinology publishes Research Highlights, Comments, News & Views, Reviews, Consensus Statements, and Perspectives relevant to researchers and clinicians in the fields of endocrinology and metabolism. Its broad scope ensures that the work it publishes reaches the widest possible audience.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


