左心室心内膜单极低电压区的范围与非缺血性心肌病室性心动过速的相关性
IF 5.6
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
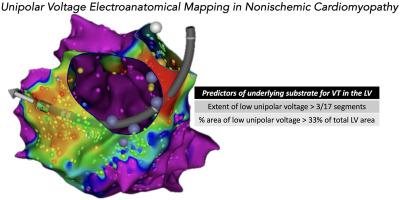
背景尚未充分探讨非缺血性心肌病(NICM)的心内膜电图(EGM)特征对预后的影响。目的我们旨在研究双极和单极 EGM 特征与 NICM 患者左室射血分数(LVEF)和室性心动过速(VT)的相关性。EGM 特征与 LVEF 相关。结果在 43 例患者中,单极 EGM 变量与基线 LVEF 的相关性优于双极 EGM 变量:单极电压(r = +0.36)、单极负电压峰值(r = -0.42)、单极正电压峰值(r = +0.38)和单极低电压区(LVZ;r = -0.41)。全球平均单极电压(危险比 [HR],0.4;95% 置信区间 [CI],0.2-0.8)、单极低压区范围(HR,1.6;95% CI,1.1-2.3)和单极低压区面积百分比(HR,1.6;95% CI,1.1-2.3)均可显著预测 VT。对于 VT 患者的分类,单极 LVZ 范围的曲线下面积为 0.82 (95% CI, 0.69-0.95; P < .001),单极 LVZ 面积百分比的曲线下面积为 0.83 (95% CI, 0.71-0.96; P = .01)。结论在 NICM 中,单极 LVZ 的范围和百分比面积是 VT 的重要预测指标。3段单极左心室区和33%单极左心室区面积的临界值与VT的相关性具有良好的诊断准确性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Correlation of extent of left ventricular endocardial unipolar low-voltage zones with ventricular tachycardia in nonischemic cardiomyopathy
Background
Endocardial electrogram (EGM) characteristics in nonischemic cardiomyopathy (NICM) have not been explored adequately for prognostication.
Objective
We aimed to study correlation of bipolar and unipolar EGM characteristics with left ventricular ejection fraction (LVEF) and ventricular tachycardia (VT) in NICM.
Methods
Electroanatomic mapping of the left ventricle was performed. EGM characteristics were correlated with LVEF. Differences between groups with and without VT and predictors of VT were studied.
Results
In 43 patients, unipolar EGM variables had better correlation with baseline LVEF than bipolar EGM variables: unipolar voltage (r = +0.36), peak negative unipolar voltage (r = −0.42), peak positive unipolar voltage (r = +0.38), and percentage area of unipolar low-voltage zone (LVZ; r = −0.41). Global mean unipolar voltage (hazard ratio [HR], 0.4; 95% confidence interval [CI], 0.2–0.8), extent of unipolar LVZ (HR, 1.6; 95% CI, 1.1–2.3), and percentage area of unipolar LVZ (HR, 1.6; 95% CI, 1.1–2.3) were significant predictors of VT. For classification of patients with VT, extent of unipolar LVZ had an area under the curve of 0.82 (95% CI, 0.69–0.95; P < .001), and percentage area of unipolar LVZ had an area under the curve of 0.83 (95% CI, 0.71–0.96; P = .01). Cutoff of >3 segments for extent of unipolar LVZ had the best diagnostic accuracy (sensitivity, 90%; specificity, 67%) and cutoff of 33% for percentage area of unipolar LVZ had the best diagnostic accuracy (sensitivity, 95%; specificity, 60%) for VT.
Conclusion
In NICM, extent and percentage area of unipolar LVZs are significant predictors of VT. Cutoffs of >3 segments of unipolar LVZ and >33% area of unipolar LVZ have good diagnostic accuracies for association with VT.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Heart rhythm
医学-心血管系统
CiteScore
10.50
自引率
5.50%
发文量
1465
审稿时长
24 days
期刊介绍:
HeartRhythm, the official Journal of the Heart Rhythm Society and the Cardiac Electrophysiology Society, is a unique journal for fundamental discovery and clinical applicability.
HeartRhythm integrates the entire cardiac electrophysiology (EP) community from basic and clinical academic researchers, private practitioners, engineers, allied professionals, industry, and trainees, all of whom are vital and interdependent members of our EP community.
The Heart Rhythm Society is the international leader in science, education, and advocacy for cardiac arrhythmia professionals and patients, and the primary information resource on heart rhythm disorders. Its mission is to improve the care of patients by promoting research, education, and optimal health care policies and standards.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


