营养不良、肌肉疏松症和恶病质:探讨癌症老年患者的患病率、重叠率和看法
IF 3.6
3区 医学
Q2 NUTRITION & DIETETICS
引用次数: 0
摘要
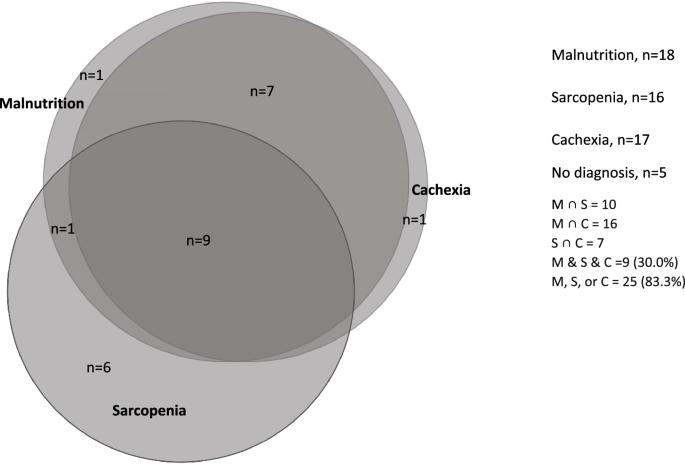
背景老年癌症患者越来越多,他们需要针对性的护理以获得最佳治疗效果。由于营养不良、肌肉疏松症和恶病质等消耗性疾病未得到充分认识和治疗,他们的护理工作变得更加复杂。我们旨在调查老年癌症患者营养不良、肌肉疏松症和恶病质的患病率、重叠率以及患者的观点和经历。通过现象学视角对访谈进行主题分析,并使用反馈回路分析法调查主题之间的关系,同时使用修改后的批判性解释综合法对调查结果进行综合。18人(60.0%)营养不良,16人(53.3%)肌肉疏松,17人(56.7%)恶病质。80%的患者有一种或多种病症,30%的患者三种病症都有。在单变量分析中,罗克伍德临床虚弱评分(OR 2.94 [95% CI:1.26-6.89,p = 0.013])与肌肉疏松症相关,报告的膳食消费百分比(OR 2.28 [95% CI:1.24-4.19,p = 0.008])与肌肉疏松症相关。19, p = 0.008])、明显消瘦(OR 8.43 [95% CI: 1.9-37.3] p = 0.005)与营养不良相关,每月体重减轻百分比(OR 8.71 [95% CI: 1.87-40.60] p = 0.006)与恶病质相关。筛查工具确定的是已确定的病症,而不是 "风险"。营养和功能问题常常被患者和临床医生(在患者看来)忽视、掩盖和误解;被错误地归因于衰老、癌症或合并症。结论:对这些疾病的认识、识别和管理都需要改进,临床医生和患者都要认识到它们的重要性,这样才能识别出真正的 "高危 "人群,同时采取更有效的干预措施。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Malnutrition, sarcopenia and cachexia: exploring prevalence, overlap, and perceptions in older adults with cancer
Older adults with cancer are a growing population requiring tailored care to achieve optimum treatment outcomes. Their care is complicated by under-recognised and under-treated wasting disorders: malnutrition, sarcopenia, and cachexia. We aimed to investigate the prevalence, overlap, and patients’ views and experiences of malnutrition, sarcopenia, and cachexia, in older adults with cancer. Mixed-methods study with cross-sectional study and qualitative interviews. Interviews were thematically analysed through a phenomenological lens, with feedback loop analysis investigating relationships between themes and findings synthesised using modified critical interpretative synthesis. n = 30 were screened for malnutrition, sarcopenia, and cachexia, n = 8 completed semi-structured interviews. Eighteen (60.0%) were malnourished, 16 (53.3%) sarcopenic, and 17 (56.7%) cachexic. One or more condition was seen in 80%, and all three in 30%. In univariate analysis, Rockwood clinical frailty score (OR 2.94 [95% CI: 1.26–6.89, p = 0.013]) was associated with sarcopenia, reported percentage meal consumption (OR 2.28 [95% CI: 1.24–4.19, p = 0.008]), and visible wasting (OR 8.43 [95% CI: 1.9–37.3] p = 0.005) with malnutrition, and percentage monthly weight loss (OR 8.71 [95% CI: 1.87–40.60] p = 0.006) with cachexia. Screening tools identified established conditions rather than ‘risk’. Nutritional and functional problems were often overlooked, overshadowed, and misunderstood by both patients and (in patients’ perceptions) by clinicians; misattributed to ageing, cancer, or comorbidities. Patients viewed these conditions as both personal impossibilities, yet accepted inevitabilities. Perceptions, identification, and management of these conditions needs to improve, and their importance recognised by clinicians and patients so those truly ‘at risk’ are identified whilst conditions are more remediable to interventions.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
10.60
自引率
2.10%
发文量
189
审稿时长
3-6 weeks
期刊介绍:
The European Journal of Clinical Nutrition (EJCN) is an international, peer-reviewed journal covering all aspects of human and clinical nutrition. The journal welcomes original research, reviews, case reports and brief communications based on clinical, metabolic and epidemiological studies that describe methodologies, mechanisms, associations and benefits of nutritional interventions for clinical disease and health promotion.
Topics of interest include but are not limited to:
Nutrition and Health (including climate and ecological aspects)
Metabolism & Metabolomics
Genomics and personalized strategies in nutrition
Nutrition during the early life cycle
Health issues and nutrition in the elderly
Phenotyping in clinical nutrition
Nutrition in acute and chronic diseases
The double burden of ''malnutrition'': Under-nutrition and Obesity
Prevention of Non Communicable Diseases (NCD)

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


