沙库比特利/缬沙坦逆转左心室重构与改善耐药性高血压患者的血液动力学有关
IF 3
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
萨库比特利/缬沙坦(S/V)已被证明是一种有效的降压药物组合。然而,它对抵抗性高血压(RHTN)患者的血压(BP)、血液动力学和左心室(LV)重塑的治疗效果仍不明确。86名患者完成了这项自我控制研究,在研究的前8周(第一阶段)服用了奥美沙坦酯,随后在后8周(第二阶段)服用了S/V,并将硝苯地平和氢氯噻嗪作为背景药物。在基线、第 8 周和第 16 周时,使用阻抗心动图进行诊室血压、超声心动图和血液动力学评估。与第一阶段相比,第二阶段的诊室血压降低幅度更大(19.59/11.66 mmHg 对 2.88/1.15 mmHg)。此外,第 2 阶段治疗对全身血管阻力指数(SVRI)和胸廓血液饱和度比值(TBR)的降低幅度更大,两个阶段的差异分别为-226.59(-1212.80 至 509.55)dyn-s/cm/m 和-0.02(-0.04 至 0.02)。从奥美沙坦转为 S/V 还能显著降低 E/E′、左心室质量指数、左心室舒张末期容积指数和左心室收缩末期容积指数(均 < 0.05)。动脉僵化、SVRI 和 TBR 的降低与 LV 重塑指标的变化相关(均<0.05)。即使在调整了包括血压变化在内的混杂因素后,这种相关性仍然存在。将奥美沙坦换成 S/V,可有效降低血压并逆转 RHTN 的心室重构。此外,还观察到血液动力学的改善。血液动力学的变化在S/V逆转左心室重构的过程中发挥了重要作用,而且与S/V的降压作用无关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
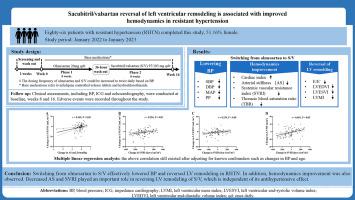

Sacubitril/valsartan reversal of left ventricular remodeling is associated with improved hemodynamics in resistant hypertension
Background
Sacubitril/valsartan (S/V) has been shown to be an effective antihypertensive drug combination. However, its therapeutic effects on blood pressure (BP), hemodynamics, and left ventricular (LV) remodeling in resistant hypertension (RHTN) remain unclear.
Methods
Eighty-six patients completed this self-control study, during which olmesartan was administered within the first 8 weeks (phase 1), followed by S/V within the second 8 weeks (phase 2), with nifedipine and hydrochlorothiazide taken as background medications. Office BP, echocardiography, and hemodynamics assessment using impedance cardiography were performed at baseline and at the eighth and sixteenth weeks.
Results
The reduction in office BP was larger in phase 2 than in phase 1 (19.59/11.66 mmHg vs. 2.88/1.15 mmHg). Furthermore, the treatment in phase 2 provided greater reductions in systemic vascular resistance index (SVRI) and thoracic blood saturation ratio (TBR), with differences between the two phases of −226.59 (−1212.80 to 509.55) dyn·s/cm5/m2 and −0.02 (−0.04 to 0.02). Switching from olmesartan to S/V also significantly reduced E/E′, LV mass index, LV end-diastolic volume index, and LV end-systolic volume index (all P < 0.05). Decreases in arterial stiffness, SVRI, and TBR were correlated with changes in indicators of LV remodeling (all P < 0.05). This correlation persisted even after adjusting for confounders including changes in BP.
Conclusions
Switching from olmesartan to S/V effectively lowered BP and reversed ventricular remodeling in RHTN. In addition, hemodynamic improvement was also observed. Changes in hemodynamics played an important role in reversing LV remodeling of S/V, and were independent of its antihypertensive effect.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Hellenic Journal of Cardiology
CARDIAC & CARDIOVASCULAR SYSTEMS-
CiteScore
4.90
自引率
7.30%
发文量
86
审稿时长
56 days
期刊介绍:
The Hellenic Journal of Cardiology (International Edition, ISSN 1109-9666) is the official journal of the Hellenic Society of Cardiology and aims to publish high-quality articles on all aspects of cardiovascular medicine. A primary goal is to publish in each issue a number of original articles related to clinical and basic research. Many of these will be accompanied by invited editorial comments.
Hot topics, such as molecular cardiology, and innovative cardiac imaging and electrophysiological mapping techniques, will appear frequently in the journal in the form of invited expert articles or special reports. The Editorial Committee also attaches great importance to subjects related to continuing medical education, the implementation of guidelines and cost effectiveness in cardiology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


