医疗保险受益人和退伍军人中新出现的转移性阉割敏感性前列腺癌种族差异
IF 5.1
2区 医学
Q1 ONCOLOGY
引用次数: 0
摘要
背景以前的研究表明,黑人男性接受的前列腺癌治疗比白人男性差。在目前的治疗时代,尚未对转移性阉割敏感性前列腺癌(mCSPC)的这一情况进行探讨。方法我们评估了Medicare(2015-2018年)和退伍军人健康管理局(VHA;2015-2019年)mCSPC患者的治疗强化(TI)和总生存率(OS),将mCSPC一线治疗分为雄激素剥夺疗法(ADT)+新型激素疗法;ADT+多西他赛;ADT+第一代非甾体抗雄激素;或单独ADT。结果我们分析了2226名黑人和16071名白人Medicare患者,以及1020名黑人和2364名白人VHA患者。总体而言,黑人与白人医疗保险患者的 TI 明显较低(调整后的比值比 [OR] 0.68;95% 置信区间 [CI]0.58-0.81),而无医疗补助患者的 TI 则明显较低(调整后的比值比 [OR] 0.70;95% 置信区间 [CI]0.57-0.87)。无论种族如何,医疗补助患者的 TI 均较低。黑人与白人医保患者的总体 OS 较差(调整后危险比 [HR] 1.20;95% CI 1.09-1.31),而非医保患者的 OS 较差(调整后危险比 1.13;95% CI 1.01-1.27)。有医疗补助与没有医疗补助的患者的 OS 较差,不同种族之间的 OS 无明显差异。黑人 VHA 患者的 TI 明显低于白人 VHA 患者(调整后 OR 0.75;95% CI 0.61-0.92),种族间 OS 无明显差异。在医疗保险计划中,黑人种族与较差的 OS 有关,但与 VHA 无关。与没有医疗补助的患者相比,医疗补助患者的 TI 更低,OS 更差,这表明贫困和种族与护理和治疗效果有关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
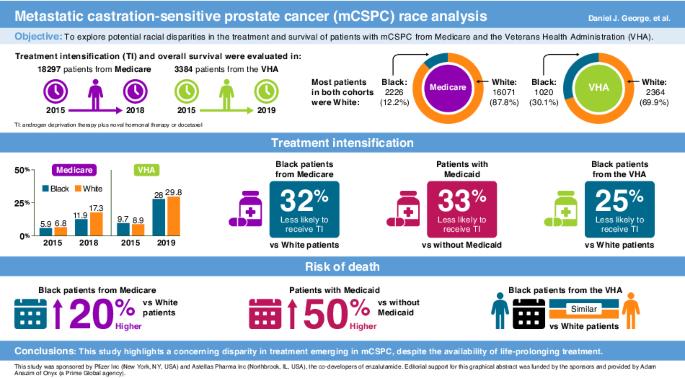
Emerging racial disparities among Medicare beneficiaries and Veterans with metastatic castration-sensitive prostate cancer
Previous studies have shown that Black men receive worse prostate cancer care than White men. This has not been explored in metastatic castration-sensitive prostate cancer (mCSPC) in the current treatment era. We evaluated treatment intensification (TI) and overall survival (OS) in Medicare (2015–2018) and Veterans Health Administration (VHA; 2015–2019) patients with mCSPC, classifying first-line mCSPC treatment as androgen deprivation therapy (ADT) + novel hormonal therapy; ADT + docetaxel; ADT + first-generation nonsteroidal antiandrogen; or ADT alone. We analyzed 2226 Black and 16,071 White Medicare, and 1020 Black and 2364 White VHA patients. TI was significantly lower for Black vs White Medicare patients overall (adjusted odds ratio [OR] 0.68; 95% confidence interval [CI] 0.58–0.81) and without Medicaid (adjusted OR 0.70; 95% CI 0.57–0.87). Medicaid patients had less TI irrespective of race. OS was worse for Black vs White Medicare patients overall (adjusted hazard ratio [HR] 1.20; 95% CI 1.09–1.31) and without Medicaid (adjusted HR 1.13; 95% CI 1.01–1.27). OS was worse in Medicaid vs without Medicaid, with no significant OS difference between races. TI was significantly lower for Black vs White VHA patients (adjusted OR 0.75; 95% CI 0.61–0.92), with no significant OS difference between races. Guideline-recommended TI was low for all patients with mCSPC, with less TI in Black patients in both Medicare and the VHA. Black race was associated with worse OS in Medicare but not the VHA. Medicaid patients had less TI and worse OS than those without Medicaid, suggesting poverty and race are associated with care and outcomes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Prostate Cancer and Prostatic Diseases
医学-泌尿学与肾脏学
CiteScore
10.00
自引率
6.20%
发文量
142
审稿时长
6-12 weeks
期刊介绍:
Prostate Cancer and Prostatic Diseases covers all aspects of prostatic diseases, in particular prostate cancer, the subject of intensive basic and clinical research world-wide. The journal also reports on exciting new developments being made in diagnosis, surgery, radiotherapy, drug discovery and medical management.
Prostate Cancer and Prostatic Diseases is of interest to surgeons, oncologists and clinicians treating patients and to those involved in research into diseases of the prostate. The journal covers the three main areas - prostate cancer, male LUTS and prostatitis.
Prostate Cancer and Prostatic Diseases publishes original research articles, reviews, topical comment and critical appraisals of scientific meetings and the latest books. The journal also contains a calendar of forthcoming scientific meetings. The Editors and a distinguished Editorial Board ensure that submitted articles receive fast and efficient attention and are refereed to the highest possible scientific standard. A fast track system is available for topical articles of particular significance.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


