通过机器学习和放射组学在 CT 扫描上对肝细胞癌微血管侵犯的术前检测:初步分析。
IF 3.5
2区 医学
Q2 ONCOLOGY
引用次数: 0
摘要
导言:微血管侵犯(MVI)是肝细胞癌(HCC)术后总死亡率和复发率的主要风险因素。研究目的是训练机器学习模型来预测术前 CT 扫描中的 MVI。DICOM 文件经过人工分割,以检测肝脏和肿瘤。从每个阶段的肿瘤区、瘤周区和健康肝区提取放射组学特征。进行主成分分析(PCA)以减少数据集的维数。数据分为训练集(70%)和测试集(30%)。随机森林(RF)、全连接 MLP 人工神经网络(neuralnet)和极梯度增强(XGB)模型被用于预测肝脏肿胀指数。结果:2008年至2022年间,共收集了218例术前CT扫描结果。在组织学标本中,72 例(33.02%)患者有 MVI。提取了一阶和二阶放射组学特征,得到了 672 个变量。在测试集中,XGB 模型的准确率为 68.7%(Sens:38.1%;Spec:83.7%;PPV:53.3%;NPV:73.4%)。神经网络的准确率为 50%(Sens:52.3%;Spec:48.8%;PPV:33.3%;NPV:67.7%)。RF 的表现最好(Acc = 96.8%,95%CI: 0.91-0.99,Sens: 95.2%,Spec:结论:我们的模型能准确预测 HCC 诊断时是否存在 MVI。结论:我们的模型对 HCC 诊断时是否存在 MVI 有很高的预测准确性,这将有助于改变这些患者的治疗分配、手术扩展和随访策略。本文章由计算机程序翻译,如有差异,请以英文原文为准。
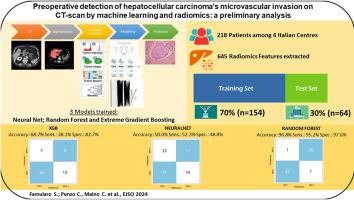

Preoperative detection of hepatocellular carcinoma's microvascular invasion on CT-scan by machine learning and radiomics: A preliminary analysis
Introduction
Microvascular invasion (MVI) is the main risk factor for overall mortality and recurrence after surgery for hepatocellular carcinoma (HCC).The aim was to train machine-learning models to predict MVI on preoperative CT scan.
Methods
3-phases CT scans were retrospectively collected among 4 Italian centers. DICOM files were manually segmented to detect the liver and the tumor(s). Radiomics features were extracted from the tumoral, peritumoral and healthy liver areas in each phase. Principal component analysis (PCA) was performed to reduce the dimensions of the dataset. Data were divided between training (70%) and test (30%) sets. Random-Forest (RF), fully connected MLP Artificial neural network (neuralnet) and extreme gradient boosting (XGB) models were fitted to predict MVI. Prediction accuracy was estimated in the test set.
Results
Between 2008 and 2022, 218 preoperative CT scans were collected. At the histological specimen, 72(33.02%) patients had MVI. First and second order radiomics features were extracted, obtaining 672 variables. PCA selected 58 dimensions explaining >95% of the variance.In the test set, the XGB model obtained Accuracy = 68.7% (Sens: 38.1%, Spec: 83.7%, PPV: 53.3% and NPV: 73.4%). The neuralnet showed an Accuracy = 50% (Sens: 52.3%, Spec: 48.8%, PPV: 33.3%, NPV: 67.7%). RF was the best performer (Acc = 96.8%, 95%CI: 0.91–0.99, Sens: 95.2%, Spec: 97.6%, PPV: 95.2% and NPV: 97.6%).
Conclusion
Our model allowed a high prediction accuracy of the presence of MVI at the time of HCC diagnosis. This could lead to change the treatment allocation, the surgical extension and the follow-up strategy for those patients.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Ejso
医学-外科
CiteScore
6.40
自引率
2.60%
发文量
1148
审稿时长
41 days
期刊介绍:
JSO - European Journal of Surgical Oncology ("the Journal of Cancer Surgery") is the Official Journal of the European Society of Surgical Oncology and BASO ~ the Association for Cancer Surgery.
The EJSO aims to advance surgical oncology research and practice through the publication of original research articles, review articles, editorials, debates and correspondence.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


