晚期房室传导异常患者的左束支区起搏与传统起搏:一项前瞻性队列研究。
IF 3
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
背景:左束支区起搏(LBBAP)是一种新兴的起搏方法,可避免右室起搏的有害影响。本研究旨在比较左束支区起搏与右室间隔起搏(RVSP)对晚期房室传导异常和左室射血分数保留患者的影响:方法:起搏的效果通过超声心动图不同步指数进行评估,包括心肌整体工作效率(GWE)和收缩峰值弥散(PSD)。主要终点是术后3个月、6个月和12个月的GWE:20名患者接受了LBBAP,18名患者接受了RVSP。由于一名患者(RVSP 组)非相关原因死亡,37 名患者(97.4%)完成了完全随访。在所有时间点上,LBBAP 组的 GWE 都明显高于 RVSP 组(12 个月时,LBBAP 组为 90.8%,RVSP 组为 85.8%,P=0.01)。在所有时间点上,LBBAP 组的 PSD 均较低,但无统计学意义(12 个月时,LBBAP 组为 56.4 毫秒,RVSP 组为 65.1 毫秒,P=0.178)。植入时间有所增加(LBBAP 组中位 93 分钟,RVSP 组中位 45 分钟,P=0.178):对于有起搏指征的患者来说,LBBAP 是一种新兴且安全的技术。尽管手术和透视时间较长,DAP也较高,但根据GWE测量结果,LBBAP与RVSP相比,似乎能提供更好的左心室同步性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Left bundle branch area pacing versus conventional pacing in patients with advanced atrioventricular conduction abnormalities: a prospective cohort study
Background
Left bundle branch area pacing (LBBAP) is an emerging pacing method that may prevent the deleterious effects of right ventricular pacing. The aim of this study is to compare the effects of LBBAP with right ventricular septal pacing (RVSP) in patients with advanced atrioventricular conduction abnormalities and preserved left ventricular ejection fraction.
Methods
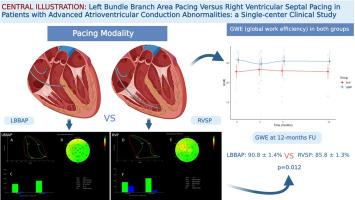
The effect of pacing was evaluated by echocardiographic indices of dyssynchrony, including global myocardial work efficiency (GWE) and peak systolic dispersion (PSD). The primary endpoint was GWE postprocedural, at 3, 6, and 12 months after the procedure.
Results
Twenty patients received LBBAP and 18 RVSP. Complete follow-up was accomplished in 37 patients (97.4%) due to the death of a patient (RVSP arm) from nonrelated cause. GWE was significantly increased in the group of LBBAP compared to RVSP at all time points (90.8% in LBBAP versus 85.8% in RVSP group at 12 months, p = 0.01). PSD was numerically lower in the LBBAP arm at all time points, yet not statistically significant (56.4 msec in LBBP versus 65.1 msec in RVSP arm at 12 months, p = 0.178). The implantation time was increased (median 93 min in LBBAP versus 45 min in RVSP group, p < 0.01), along with fluoroscopy time and dose area product (DAP), in the arm of LBBAP. There were no severe perioperative acute complications in either group.
Conclusions
LBBAP is an emerging and safe technique for patients with a pacing indication. Despite the longer procedural and fluoroscopy time, as well as higher DAP, LBBAP seems to offer better left ventricular synchrony compared to RVSP, according to GWE measurements.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Hellenic Journal of Cardiology
CARDIAC & CARDIOVASCULAR SYSTEMS-
CiteScore
4.90
自引率
7.30%
发文量
86
审稿时长
56 days
期刊介绍:
The Hellenic Journal of Cardiology (International Edition, ISSN 1109-9666) is the official journal of the Hellenic Society of Cardiology and aims to publish high-quality articles on all aspects of cardiovascular medicine. A primary goal is to publish in each issue a number of original articles related to clinical and basic research. Many of these will be accompanied by invited editorial comments.
Hot topics, such as molecular cardiology, and innovative cardiac imaging and electrophysiological mapping techniques, will appear frequently in the journal in the form of invited expert articles or special reports. The Editorial Committee also attaches great importance to subjects related to continuing medical education, the implementation of guidelines and cost effectiveness in cardiology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


