24 小时动态血压监测中的节律成分在对合并心血管疾病的慢性肾病患者进行风险分层时的预后作用
IF 2.7
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
摘要
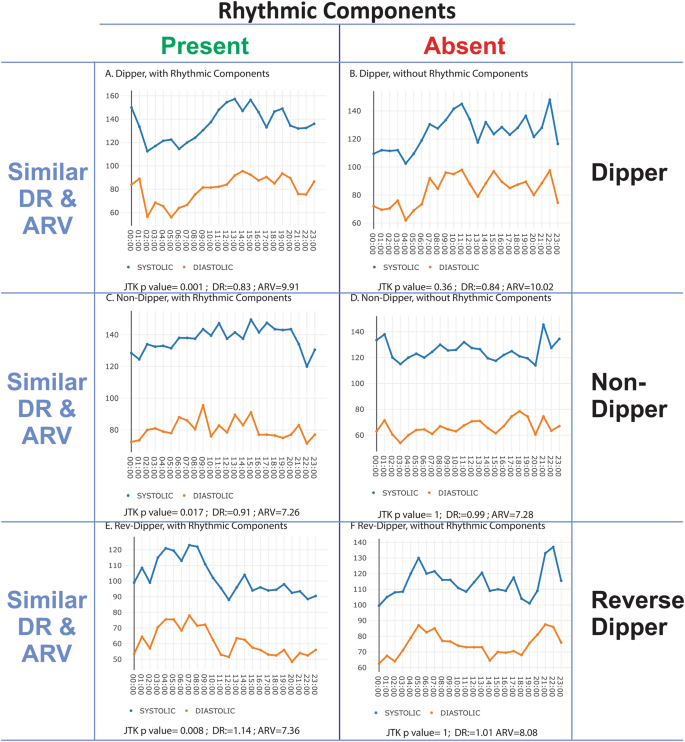
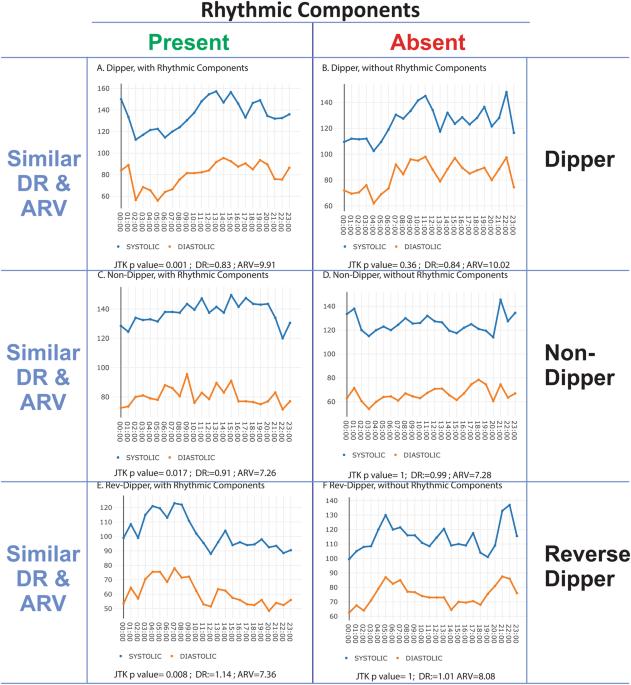
慢性肾脏病(CKD)给全球带来沉重负担。高血压是导致 CKD 快速恶化的一个可改变的风险因素。我们通过使用 Cox 比例危险模型,在慢性肾功能不全队列(CRIC)和非裔美国人肾脏病和高血压研究(AASK)队列中,采用非参数方法确定非卧床血压监测(ABPM)24 小时曲线中的节律成分,从而扩展了风险分层。我们发现,通过 JTK_CYCLE 分析对血压进行节律性分析,可以发现 CRIC 参与者中更有可能死于心血管疾病的亚组。我们的完全调整模型显示,在整个 CRIC 队列中,不存在周期性成分与心血管死亡之间存在显著联系(HR:1.71,95% CI:0.99-2.97, p = 0.056)。056),有心血管疾病(CVD)病史且血压曲线中不存在循环成分的 CRIC 参与者在任何时候的心血管死亡风险都比血压曲线中存在循环成分的 CVD 患者高 3.4 倍(HR:3.37,95% CI:1.45-7.87,p = 0.005)。ABPM 中的浸渍或非浸渍模式无法解释风险增加的原因。由于患者特征差异较大,研究结果无法在 AASK 队列中复制。这项研究表明,节律性血压成分是一种潜在的新型生物标记物,可揭示既往患有心血管疾病的慢性肾脏病患者的超常风险。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Prognostic utility of rhythmic components in 24-h ambulatory blood pressure monitoring for the risk stratification of chronic kidney disease patients with cardiovascular co-morbidity
Chronic kidney disease (CKD) represents a significant global burden. Hypertension is a modifiable risk factor for rapid progression of CKD. We extend the risk stratification by introducing the non-parametric determination of rhythmic components in 24-h profiles of ambulatory blood pressure monitoring (ABPM) in the Chronic Renal Insufficiency Cohort (CRIC) and the African American Study for Kidney Disease and Hypertension (AASK) cohort using Cox proportional hazards models. We find that rhythmic profiling of BP through JTK_CYCLE analysis identifies subgroups of CRIC participants that were more likely to die due to cardiovascular causes. While our fully adjusted model shows a trend towards a significant association between absent cyclic components and cardiovascular death in the full CRIC cohort (HR: 1.71,95% CI: 0.99–2.97, p = 0.056), CRIC participants with a history of cardiovascular disease (CVD) and absent cyclic components in their BP profile had at any time a 3.4-times higher risk of cardiovascular death than CVD patients with cyclic components present in their BP profile (HR: 3.37, 95% CI: 1.45–7.87, p = 0.005). This increased risk was not explained by the dipping or non-dipping pattern in ABPM. Due to the large differences in patient characteristics, the results do not replicate in the AASK cohort. This study suggests rhythmic blood pressure components as a potential novel biomarker to unmask excess risk among CKD patients with prior cardiovascular disease.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


