癌症阴茎患者行电视内窥镜腹股沟淋巴结切除术(VEIL)后的长期肿瘤和手术结果。
IF 3.1
3区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 3
摘要
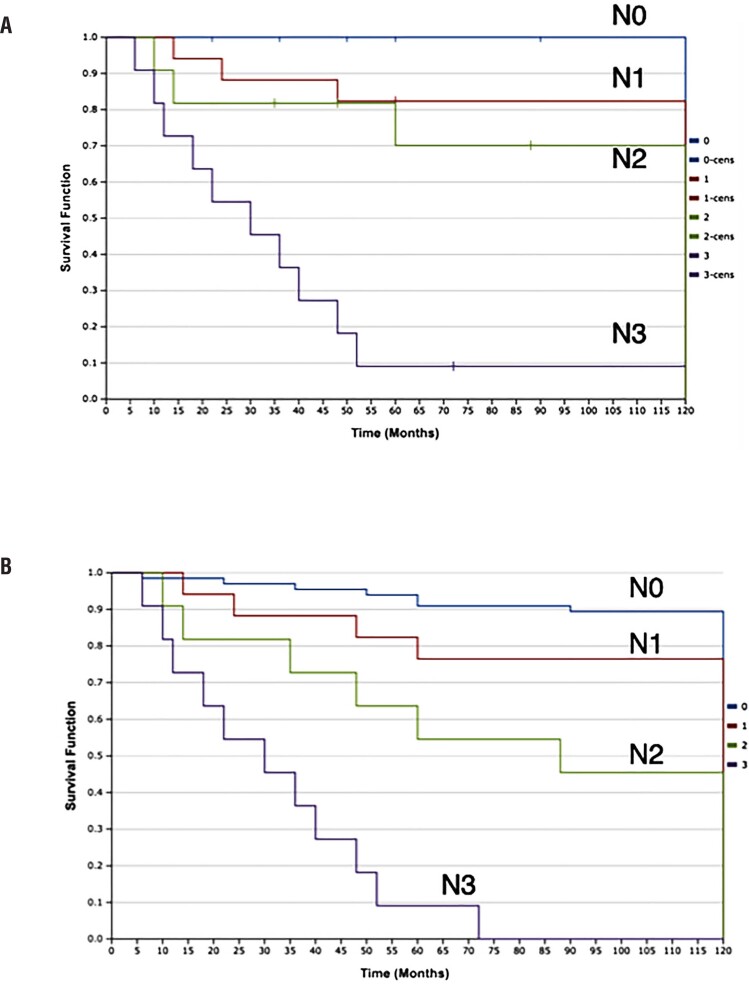
目的:报告癌症阴茎最大的多中心系列患者接受视频内窥镜腹股沟淋巴结切除术(VEIL)的结果。材料和方法:回顾性多中心分析。来自癌症合作拉丁美洲(PeC-LA)的21个中心的作者被包括在内。所有中心都按照之前描述的相同标准化技术进行手术。纳入标准包括没有可触及的淋巴结和中/高危疾病的阴茎癌症患者,以及直径小于4厘米的非固定可触及淋巴结的患者。类别变量显示为百分比和频率,而连续变量显示为平均值和范围。结果:从2006年到2020年,共对105名患者进行了210次VEIL手术。平均年龄58岁(45-68岁)。平均手术时间为90分钟(60~120分钟)。平均淋巴结产量为10个淋巴结(6-16个)。并发症发生率为15.7%,其中严重并发症发生率1.9%。淋巴结和皮肤并发症分别发生在8.6%和4.8%的患者中。组织病理学分析显示26.7%的淋巴结未触及的患者有淋巴结受累。2.8%的患者出现腹股沟复发。10年总生存率为74.2%,10年癌症特异性生存率为84.8%。pN0、pN1、pN2和pN3的CSS分别为100%、82.4%、72.7%和9.1%。结论:VEIL似乎能以最低的发病率提供适当的长期肿瘤学控制。在缺乏动态前哨淋巴结活检等非侵入性分层措施的情况下,VEIL成为癌症阴茎非体积淋巴结的替代治疗方法。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Long-term oncological and surgical outcomes after Video Endoscopic Inguinal Lymphadenectomy (VEIL) in patients with penile cancer.
ABSTRACT Objective: To report outcomes from the largest multicenter series of penile cancer patients undergoing video endoscopic inguinal lymphadenectomy (VEIL). Materials and Methods: Retrospective multicenter analysis. Authors of 21 centers from the Penile Cancer Collaborative Coalition-Latin America (PeC-LA) were included. All centers performed the procedure following the same previously described standardized technique. Inclusion criteria included penile cancer patients with no palpable lymph nodes and intermediate/high-risk disease and those with non-fixed palpable lymph nodes less than 4 cm in diameter. Categorical variables are shown as percentages and frequencies whereas continuous variables as mean and range. Results: From 2006 to 2020, 210 VEIL procedures were performed in 105 patients. Mean age was 58 (45-68) years old. Mean operative time was 90 minutes (60-120). Mean lymph node yield was 10 nodes (6-16). Complication rate was 15.7%, including severe complications in 1.9% of procedures. Lymphatic and skin complications were noted in 8.6 and 4.8% of patients, respectively. Histopathological analysis revealed lymph node involvement in 26.7% of patients with non-palpable nodes. Inguinal recurrence was observed in 2.8% of patients. 10y- overall survival was 74.2% and 10-y cancer specific survival was 84.8%. CSS for pN0, pN1, pN2 and pN3 were 100%, 82.4%, 72.7% and 9.1%, respectively. Conclusion: VEIL seems to offer appropriate long term oncological control with minimal morbidity. In the absence of non-invasive stratification measures such as dynamic sentinel node biopsy, VEIL emerged as the alternative for the management of non-bulky lymph nodes in penile cancer.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

International Braz J Urol
UROLOGY & NEPHROLOGY-
CiteScore
4.60
自引率
21.60%
发文量
246
审稿时长
6-12 weeks
期刊介绍:
Information not localized
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


